Back
Poster, Podium & Video Sessions
Moderated Poster
MP09: Prostate Cancer: Detection & Screening I
MP09-18: Longitudinal Outcomes Following Implementation of Baseline PSA Risk Stratification of Men in Their Forties
Friday, May 13, 2022
10:30 AM – 11:45 AM
Location: Room 222
Zoe Michael*, Srinath Kotamarti, Rohith Arcot, Kostantinos Morris, Anand Shah, John Anderson, Andrew Armstrong, Rajan Gupta, Glenn M. Preminger, Judd W. Moul, Kevin Oeffinger, Kevin Shah, Thomas J. Polascik, Durham, NC

Zoe D. Michael, BS,MS
Duke University
Poster Presenter(s)
Introduction: A baseline prostate-specific antigen (PSA) in a man’s forties can assess risk for lethal prostate cancer (PCa) at a time in life when PSA should be low with few confounders. We examined the initial longitudinal outcomes of young men with an elevated baseline PSA screened within a system-wide primary care network.
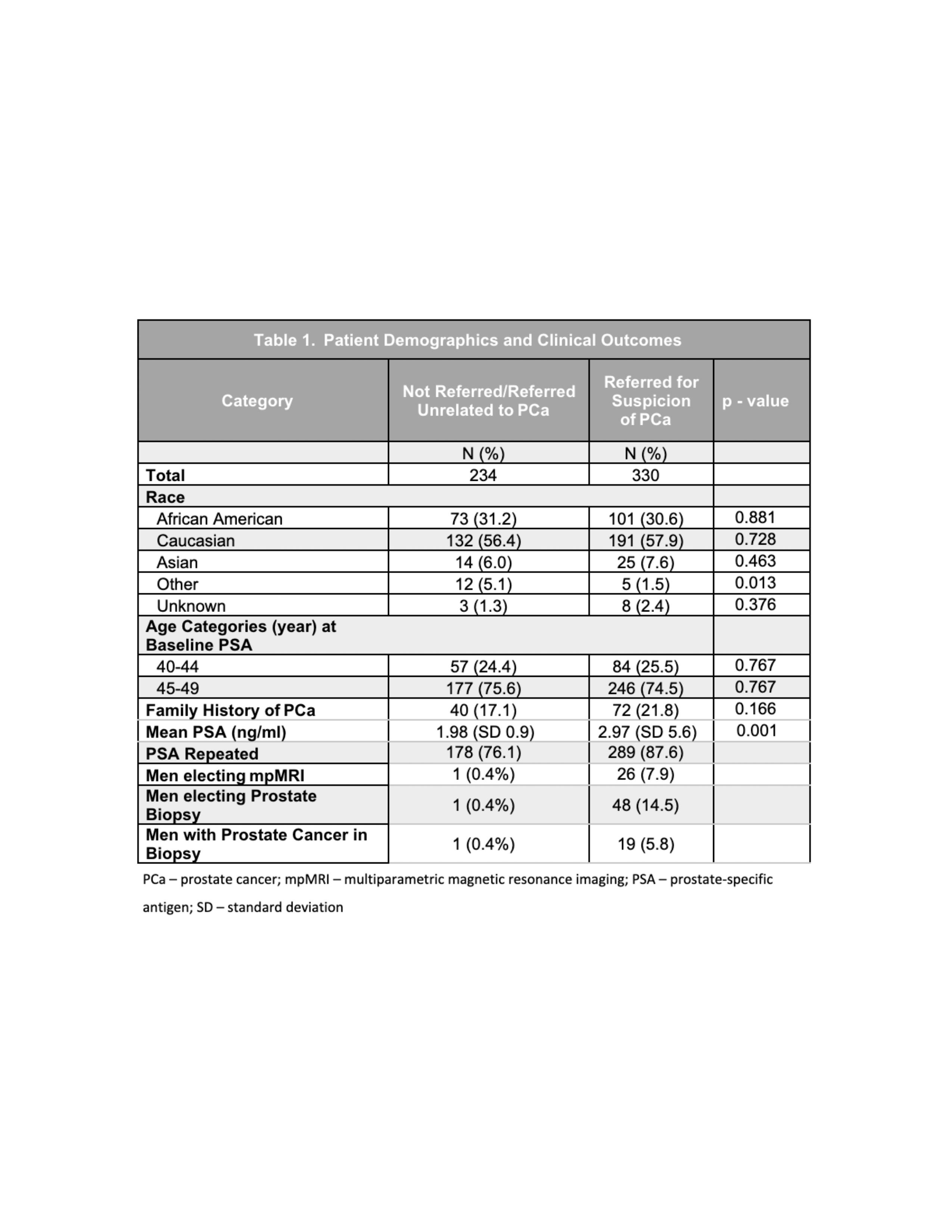
Methods: We assessed patients within the Duke Primary Care Network ages 40-49 with a PSA following implementation of an electronic health record (EHR) screening algorithm on 2/2/2017. The outcomes of men with PSA > 1.5 ng/ml were assessed through 7/2021. Statistical analyses compared mean PSAs between groups and identified factors associated with the detection of all PCa and clinically significant PCa (csPCa), defined as Gleason Grade Group (GGG) > 2.
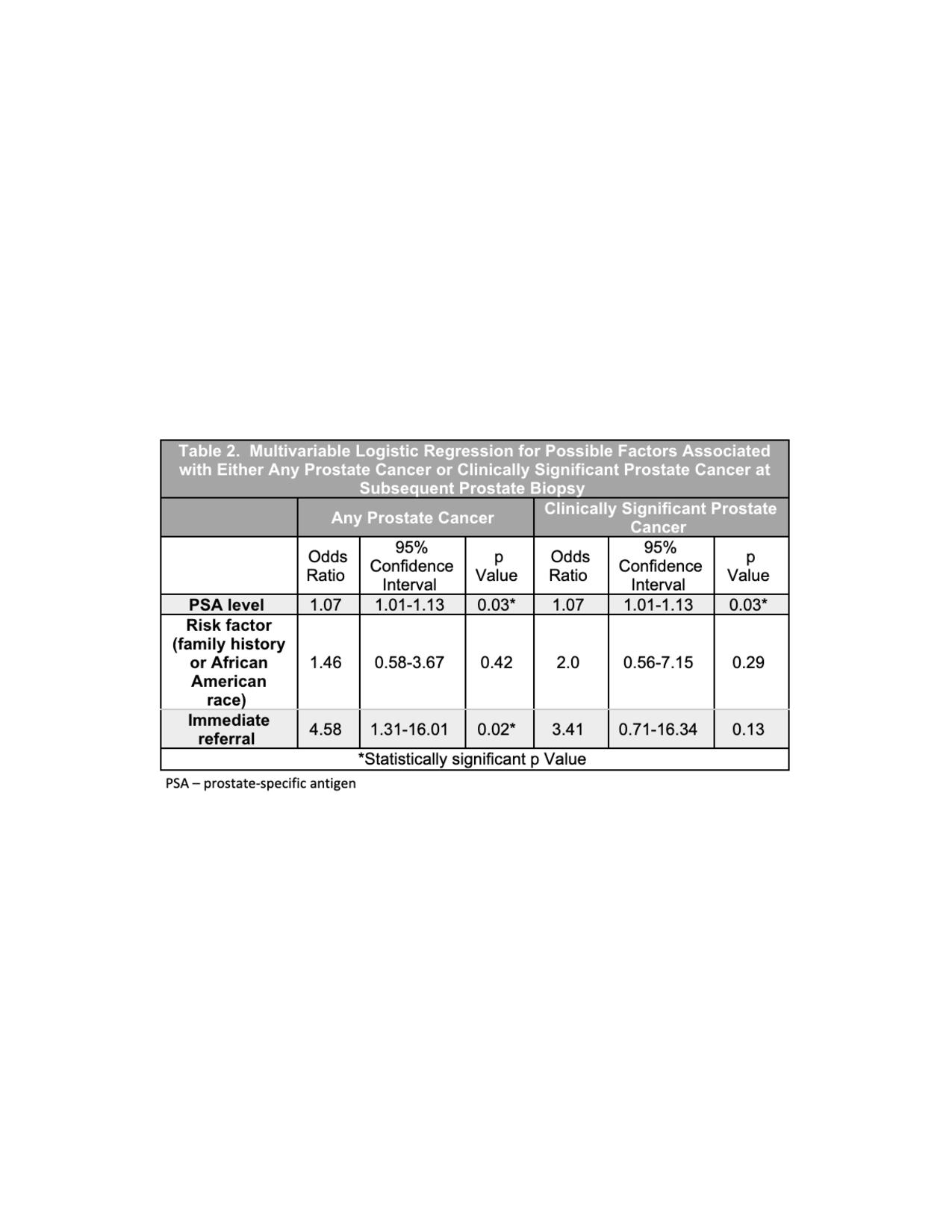
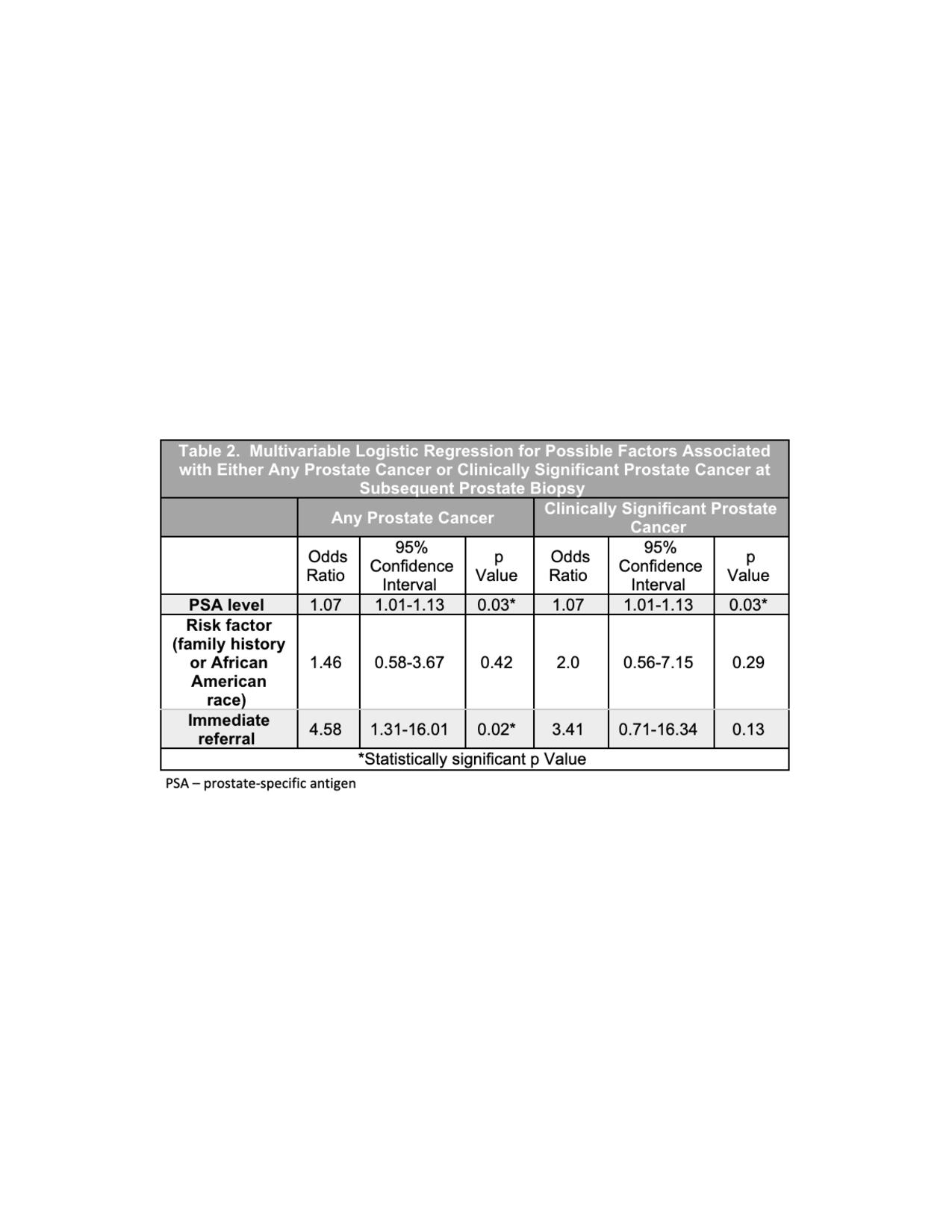
Results: Of 49,980 men screened, 11,922 men were ages 40-49, with 564 (4.7%) found to have a PSA > 1.5 ng/ml. A total of 330 (58.5%) men were referred to urology for PCa suspicion, while the remaining 234 (41.5%) were either not referred to urology (n=206) or were referred for reasons unrelated to PCa suspicion (n=28). Referred patients had significantly higher mean PSA values (2.97 vs 1.98, p=0.001). In the entire cohort, 49 patients (8.7%) underwent biopsy; of these, 20 (40.8%) returned positive for PCa. A total of 11 men had csPCa, including three patients with > GGG4. Timing of referral and PSA levels were significantly associated with all PCa at biopsy on multivariable analysis. However, a separate analysis for csPCa showed PSA was a significant predictor (OR 1.065, p<0.05), while referral timing was not (p>0.05).
Conclusions: A PSA > 1.5 ng/ml led to PCa diagnosis in a small but important percentage of men in their forties. Overall, this study provides validation for a baseline PSA measurement in younger men to determine those patients harboring lethal cancer who could benefit from potentially lifesaving intervention. Further work is needed to enhance PCP buy-in and optimize coordination between PCPs and urologists to further improve patient care.
Source of Funding: Grants from the National Cancer Institute and the Duke Institute for Health Innovation (DIHI)
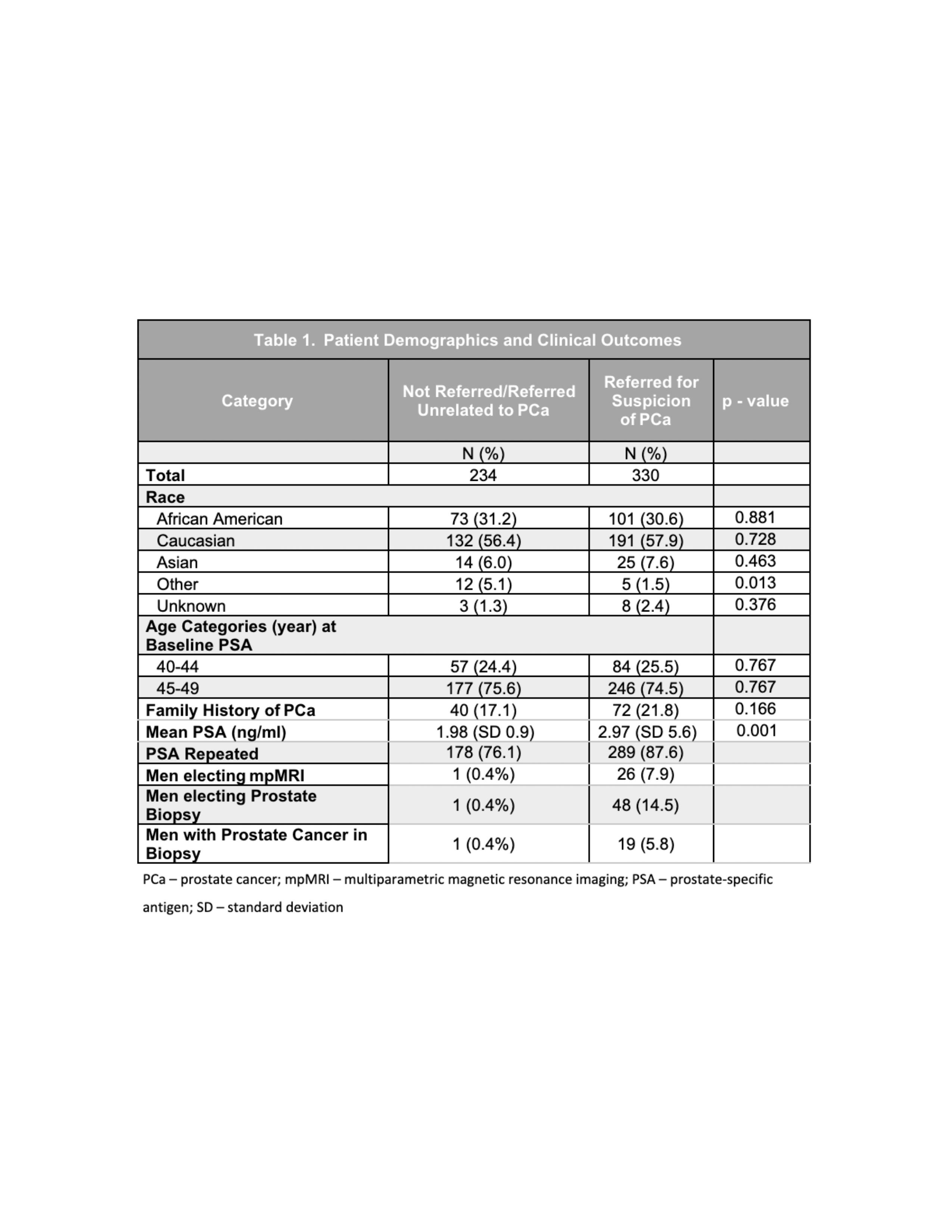
Methods: We assessed patients within the Duke Primary Care Network ages 40-49 with a PSA following implementation of an electronic health record (EHR) screening algorithm on 2/2/2017. The outcomes of men with PSA > 1.5 ng/ml were assessed through 7/2021. Statistical analyses compared mean PSAs between groups and identified factors associated with the detection of all PCa and clinically significant PCa (csPCa), defined as Gleason Grade Group (GGG) > 2.
Results: Of 49,980 men screened, 11,922 men were ages 40-49, with 564 (4.7%) found to have a PSA > 1.5 ng/ml. A total of 330 (58.5%) men were referred to urology for PCa suspicion, while the remaining 234 (41.5%) were either not referred to urology (n=206) or were referred for reasons unrelated to PCa suspicion (n=28). Referred patients had significantly higher mean PSA values (2.97 vs 1.98, p=0.001). In the entire cohort, 49 patients (8.7%) underwent biopsy; of these, 20 (40.8%) returned positive for PCa. A total of 11 men had csPCa, including three patients with > GGG4. Timing of referral and PSA levels were significantly associated with all PCa at biopsy on multivariable analysis. However, a separate analysis for csPCa showed PSA was a significant predictor (OR 1.065, p<0.05), while referral timing was not (p>0.05).
Conclusions: A PSA > 1.5 ng/ml led to PCa diagnosis in a small but important percentage of men in their forties. Overall, this study provides validation for a baseline PSA measurement in younger men to determine those patients harboring lethal cancer who could benefit from potentially lifesaving intervention. Further work is needed to enhance PCP buy-in and optimize coordination between PCPs and urologists to further improve patient care.
Source of Funding: Grants from the National Cancer Institute and the Duke Institute for Health Innovation (DIHI)

.jpg)
.jpg)