Back
Poster, Podium & Video Sessions
Best Poster Award
MP10: Education Research I
MP10-02: Urology Resident Autonomy Compared to General Surgery Resident Autonomy
Friday, May 13, 2022
1:00 PM – 2:15 PM
Location: Room 228
Kunj Jain*, Totowa, NJ, Janmejay Hingu, Anh Nguyen, Devashish Anjaria, Joseph B. Oliver, Hossein Sadeghi-Nejad, Newark, NJ

Kunj Jain, BA
Rutgers New Jersey Medical School
Poster Presenter(s)
Introduction: Urology and general surgery resident autonomy in the operating room has been declining in recent years. This may be due to perceptions of poorer outcomes, complications, and operating time. Residents and faculty have expressed decreased preparedness as independent surgeons due to inadequate autonomy during residency. We sought to compare resident involvement for general surgery and urology residents and evaluated the associated outcomes.
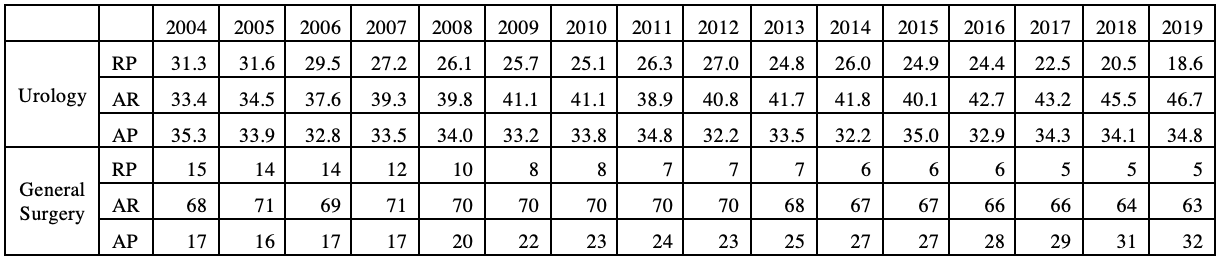
Methods: This study is a retrospective study from the Veterans Affairs Surgical Quality Improvement Program (VASQIP) database. All operative cases from July 1, 2004 to September 30, 2019 in the VASQIP database were included in the study. Patients who underwent a urologic surgical procedure were identified based on the code of the surgeon’s specialty and stratified based on CPT codes. The cases were coded based on the level of supervision by an attending physician: AP- attending as primary surgeon, RP- resident as primary surgeon, AR- attending and resident as primary surgeons. Logistic regression and ANOVA analysis was performed.
Results: The VASQIP database included 127,757 patients who underwent urologic surgery over the 15 year time frame. There was decline in resident primary surgeon (RP) cases from 31.3% in 2004 to 18.6% in 2019 with an increase in total cases (p < 0.01). The number of urology RP cases is higher compared to general surgery/vascular surgery RP cases which decreased from 15% to 5% in the same period. Urology and general surgery AR cases had increased operating times, but RP surgeries did not have significantly increased operating times when compared to AP surgeries. There was no increase in mortality with RP or AR urology cases. However, the 30-day return to OR was significantly increased compared to AP cases. There was no difference in mortality between RP or AP general surgery cases, but AP general surgery cases had an increased rate of complications.
Conclusions: Residents in urology and general surgery have had a major decline in resident autonomy between 2004 and 2019. Although urology has had better autonomy maintenance compared to general surgery, both specialties have seen a decline that is not warranted based on operating time, complications, and patient outcomes. There is a need for increased efforts to expand resident autonomy to create prepared and independent future surgeons.
Source of Funding: N/A
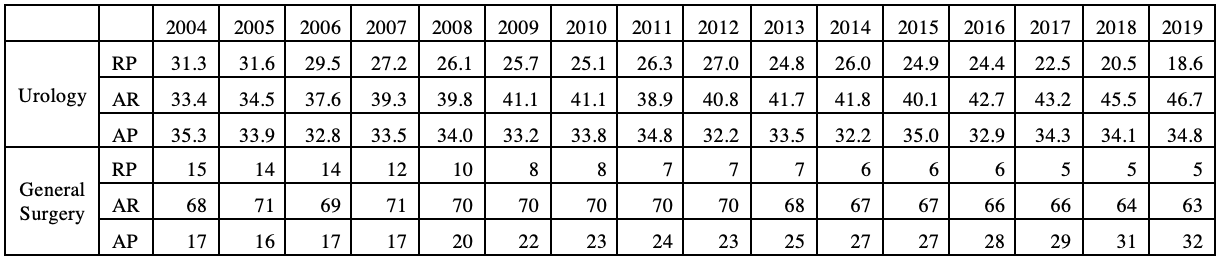
Methods: This study is a retrospective study from the Veterans Affairs Surgical Quality Improvement Program (VASQIP) database. All operative cases from July 1, 2004 to September 30, 2019 in the VASQIP database were included in the study. Patients who underwent a urologic surgical procedure were identified based on the code of the surgeon’s specialty and stratified based on CPT codes. The cases were coded based on the level of supervision by an attending physician: AP- attending as primary surgeon, RP- resident as primary surgeon, AR- attending and resident as primary surgeons. Logistic regression and ANOVA analysis was performed.
Results: The VASQIP database included 127,757 patients who underwent urologic surgery over the 15 year time frame. There was decline in resident primary surgeon (RP) cases from 31.3% in 2004 to 18.6% in 2019 with an increase in total cases (p < 0.01). The number of urology RP cases is higher compared to general surgery/vascular surgery RP cases which decreased from 15% to 5% in the same period. Urology and general surgery AR cases had increased operating times, but RP surgeries did not have significantly increased operating times when compared to AP surgeries. There was no increase in mortality with RP or AR urology cases. However, the 30-day return to OR was significantly increased compared to AP cases. There was no difference in mortality between RP or AP general surgery cases, but AP general surgery cases had an increased rate of complications.
Conclusions: Residents in urology and general surgery have had a major decline in resident autonomy between 2004 and 2019. Although urology has had better autonomy maintenance compared to general surgery, both specialties have seen a decline that is not warranted based on operating time, complications, and patient outcomes. There is a need for increased efforts to expand resident autonomy to create prepared and independent future surgeons.
Source of Funding: N/A

.jpg)
.jpg)