Back
Poster, Podium & Video Sessions
Moderated Poster
MP10: Education Research I
MP10-12: A Quality Improvement Study of Resident & Fellow Experience with Urinary Catheter Insertion
Friday, May 13, 2022
1:00 PM – 2:15 PM
Location: Room 228
Peris Castaneda*, Jenna Stelmar, Shannon Smith, Aurash Naser-Tavakolian, Maurice Garcia, Los Angeles, CA
- PC
Peris Rose Castaneda, MD
Resident Physician
Cedars-Sinai Medical Center, Department of Surgery, Division of Urology
Poster Presenter(s)
Introduction: Between 15 and 25% of patients receive indwelling urinary catheters during their hospital stay. Despite the prevalence of urinary catheterization, many physicians do not feel comfortable inserting a urinary catheter. We posit that comfort with catheter placement is related to provider specialty and training; however, this phenomenon is not well described in the medical literature. We aim to compare catheter placement training, experience, and confidence among residents and fellows of different specialties.
Methods: A survey querying catheter insertion experience, confidence and source of training was sent to residency program directors at our academic training hospital and distributed to residents and fellows. Responses were collecting using Qualtrics survey platform.
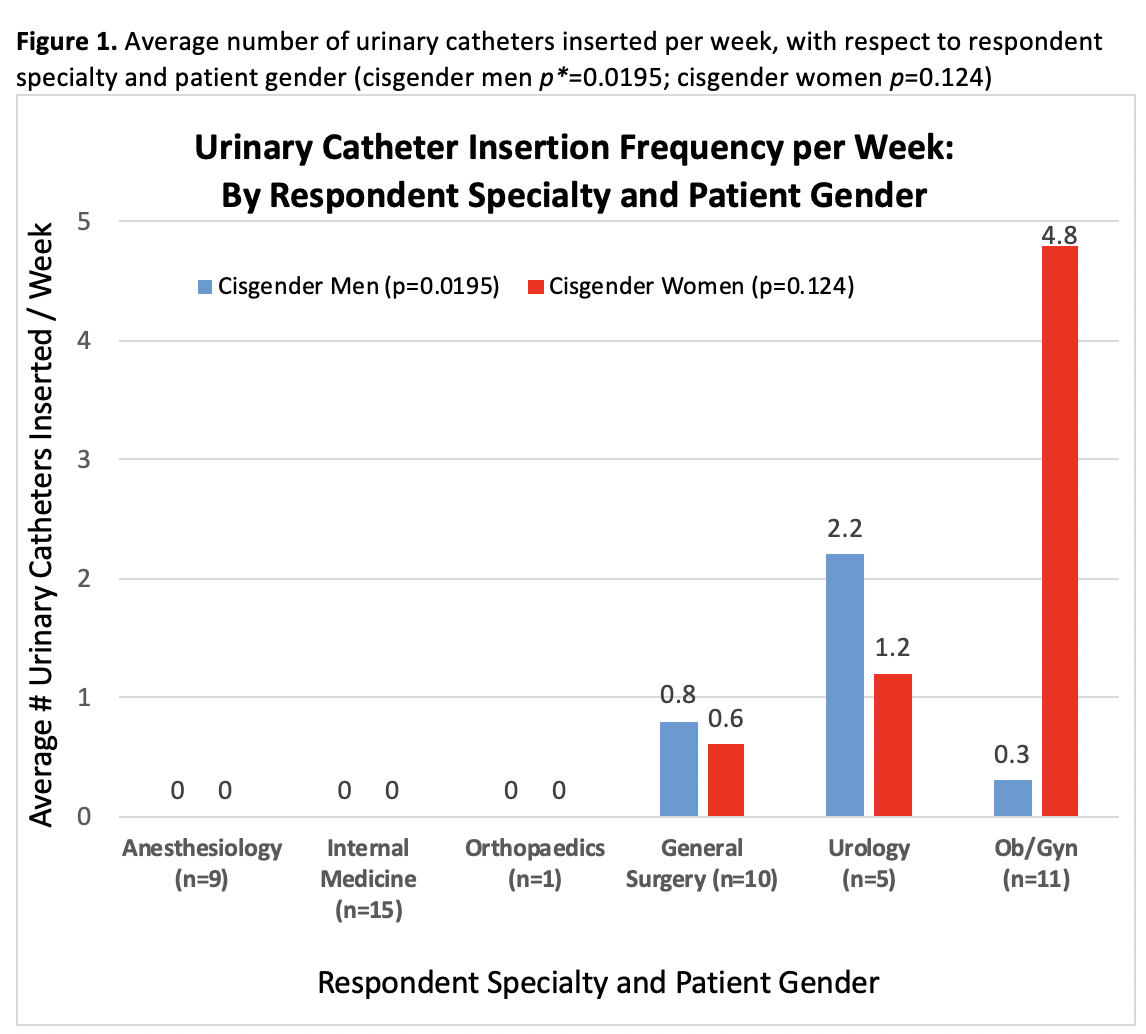
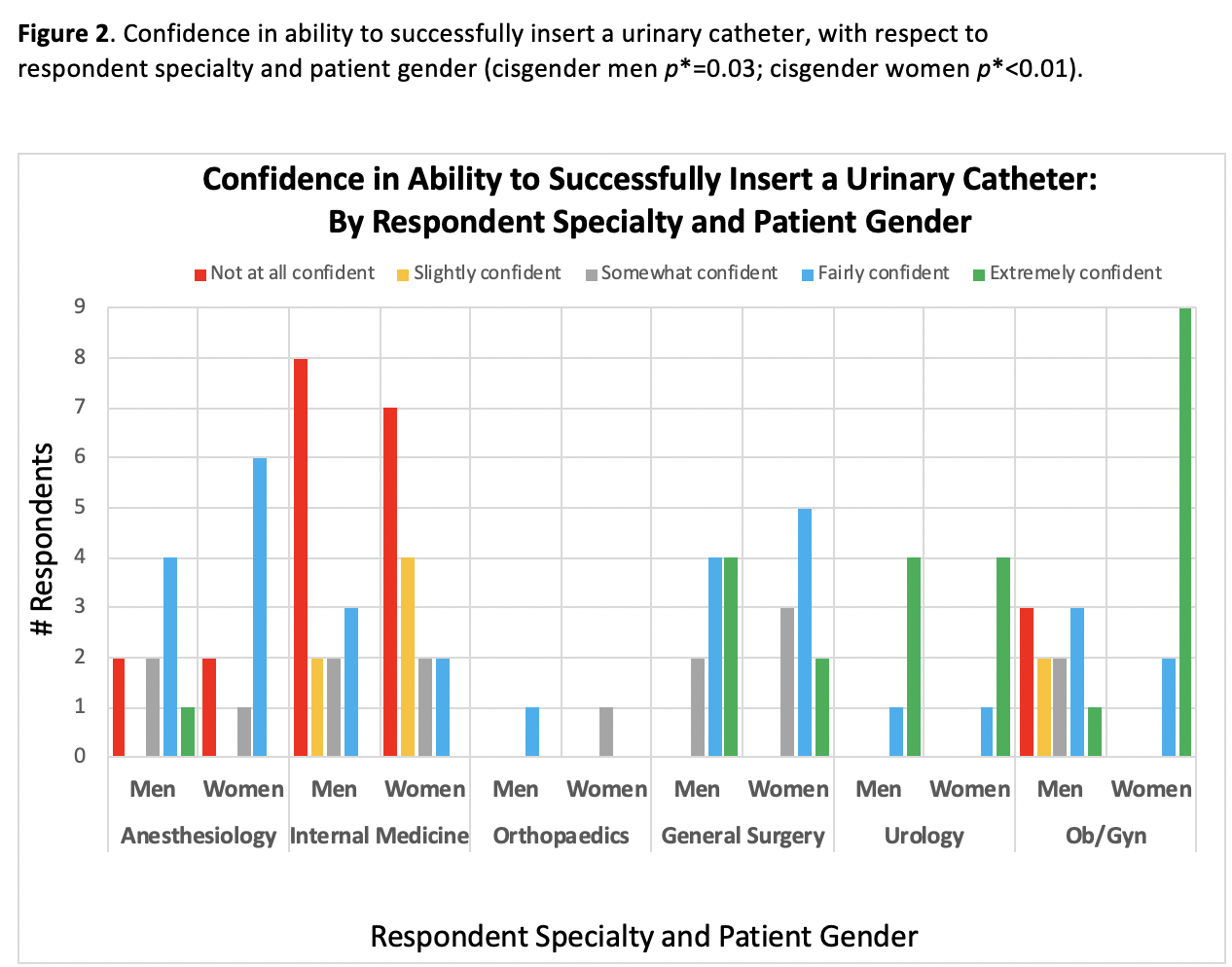
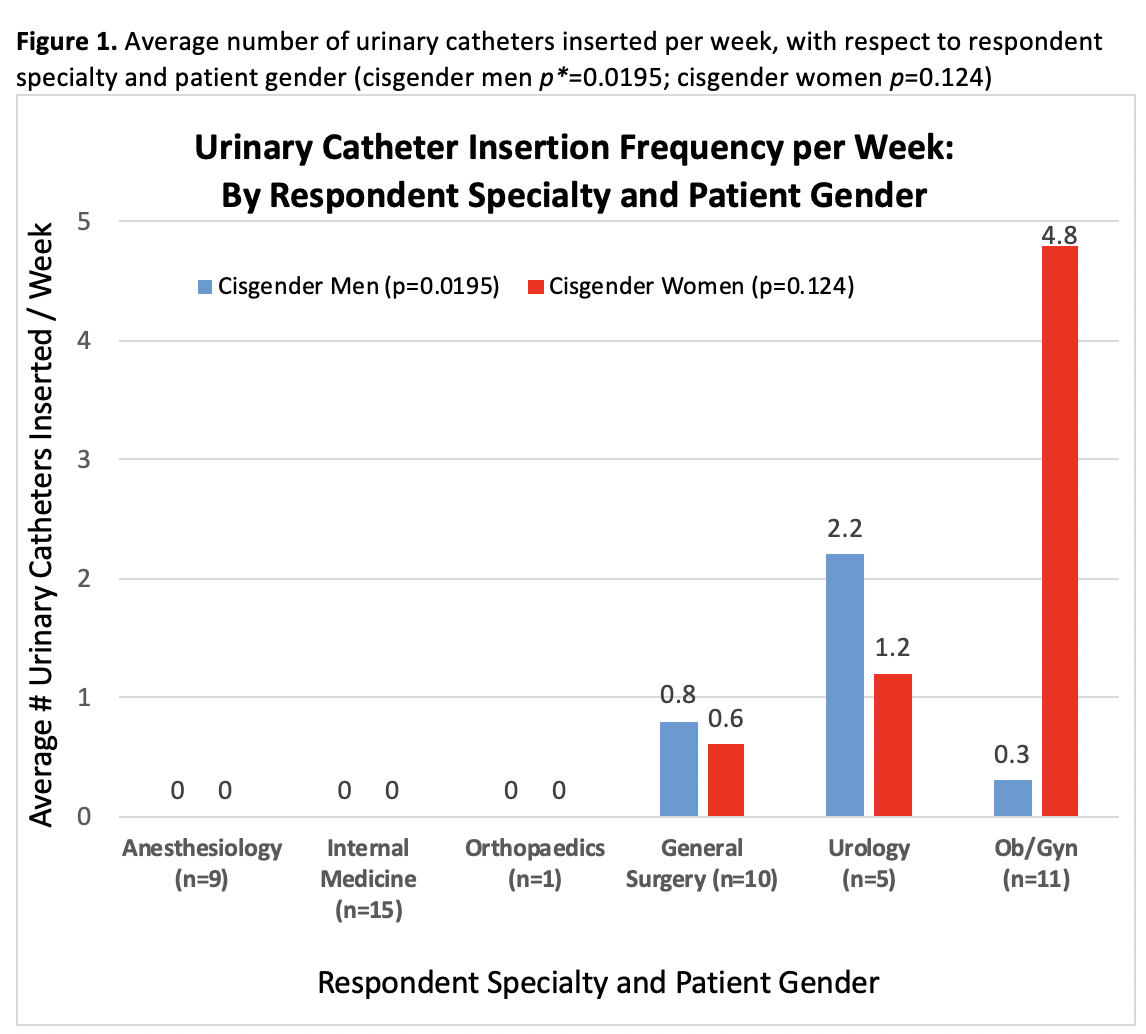
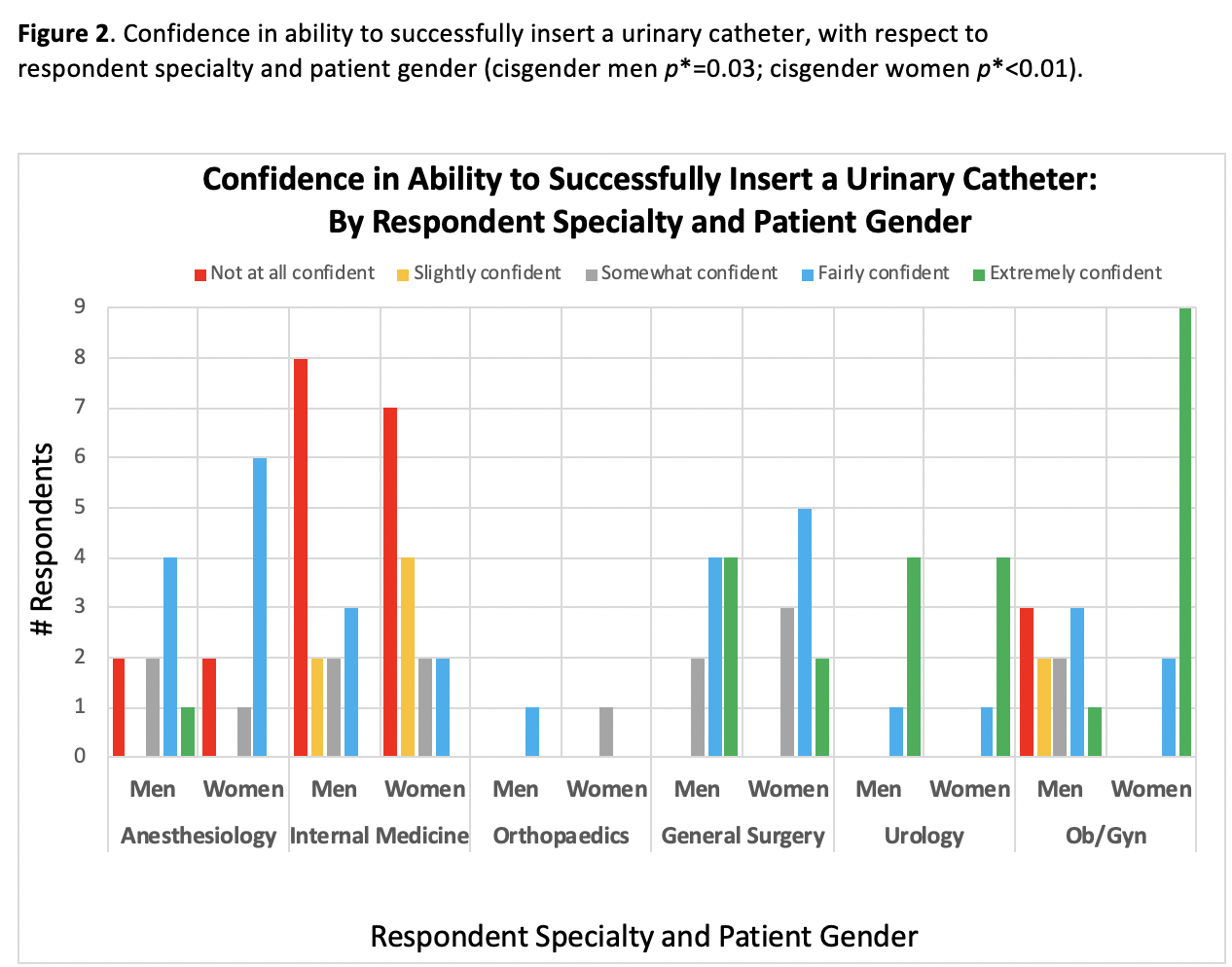
Results: Fifty-one in-training physicians completed the survey, including 11 interns, 34 residents, and 6 fellows. Six surgical and medical specialties were represented. Most trainees indicated that they learned catheter insertion from a resident (51%) and/or from a registered nurse (41%). Few trainees said they learned insertion from an attending (18%) or from a professional instructor (16%). Across all specialties, the number of catheters inserted varied significantly, and among Medicine, Anesthesiology and Ortho residents equaled zero (Figure 1). There were significant differences in trainees’ confidence in their ability to successfully insert a urinary catheter into a cisgender man (p= 0.03) and cisgender woman (p < 0.01), by specialty (Figure 2). Ob/Gyn trainees were highly confident in catheter insertion in women, but indicated lower confidence with insertion in men.
Conclusions: Resident trainees in only select surgical specialties ever insert urinary catheters; residents from other specialties reported inserting none. Few trainees learn insertion from an attending. This data suggests reconsideration of whether or not catheter insertion technique and safety should be a teaching priority for physicians and/or nurses.
Source of Funding: The Richard Onofrio research grant to the Cedars-Sinai Transgender Surgery and Health Program
Methods: A survey querying catheter insertion experience, confidence and source of training was sent to residency program directors at our academic training hospital and distributed to residents and fellows. Responses were collecting using Qualtrics survey platform.
Results: Fifty-one in-training physicians completed the survey, including 11 interns, 34 residents, and 6 fellows. Six surgical and medical specialties were represented. Most trainees indicated that they learned catheter insertion from a resident (51%) and/or from a registered nurse (41%). Few trainees said they learned insertion from an attending (18%) or from a professional instructor (16%). Across all specialties, the number of catheters inserted varied significantly, and among Medicine, Anesthesiology and Ortho residents equaled zero (Figure 1). There were significant differences in trainees’ confidence in their ability to successfully insert a urinary catheter into a cisgender man (p= 0.03) and cisgender woman (p < 0.01), by specialty (Figure 2). Ob/Gyn trainees were highly confident in catheter insertion in women, but indicated lower confidence with insertion in men.
Conclusions: Resident trainees in only select surgical specialties ever insert urinary catheters; residents from other specialties reported inserting none. Few trainees learn insertion from an attending. This data suggests reconsideration of whether or not catheter insertion technique and safety should be a teaching priority for physicians and/or nurses.
Source of Funding: The Richard Onofrio research grant to the Cedars-Sinai Transgender Surgery and Health Program

.jpg)
.jpg)