Back
Poster, Podium & Video Sessions
Moderated Poster
MP10: Education Research I
MP10-16: Interactive Online Urology Curriculum for Medical Students: A Multi-Institutional Pilot Study
Friday, May 13, 2022
1:00 PM – 2:15 PM
Location: Room 228
Ezra Margolin*, Jane Kurtzman, Rachel Gordon, Christopher Anderson, Gina Badalato, New York, NY

Ezra J. Margolin, MD
Columbia University
Poster Presenter(s)
Introduction: The role of interactive online learning tools in medical education has expanded in multiple disciplines but is still absent in urology. We sought to develop and evaluate an interactive online urology curriculum for medical students, to be used at a multi-institutional level.
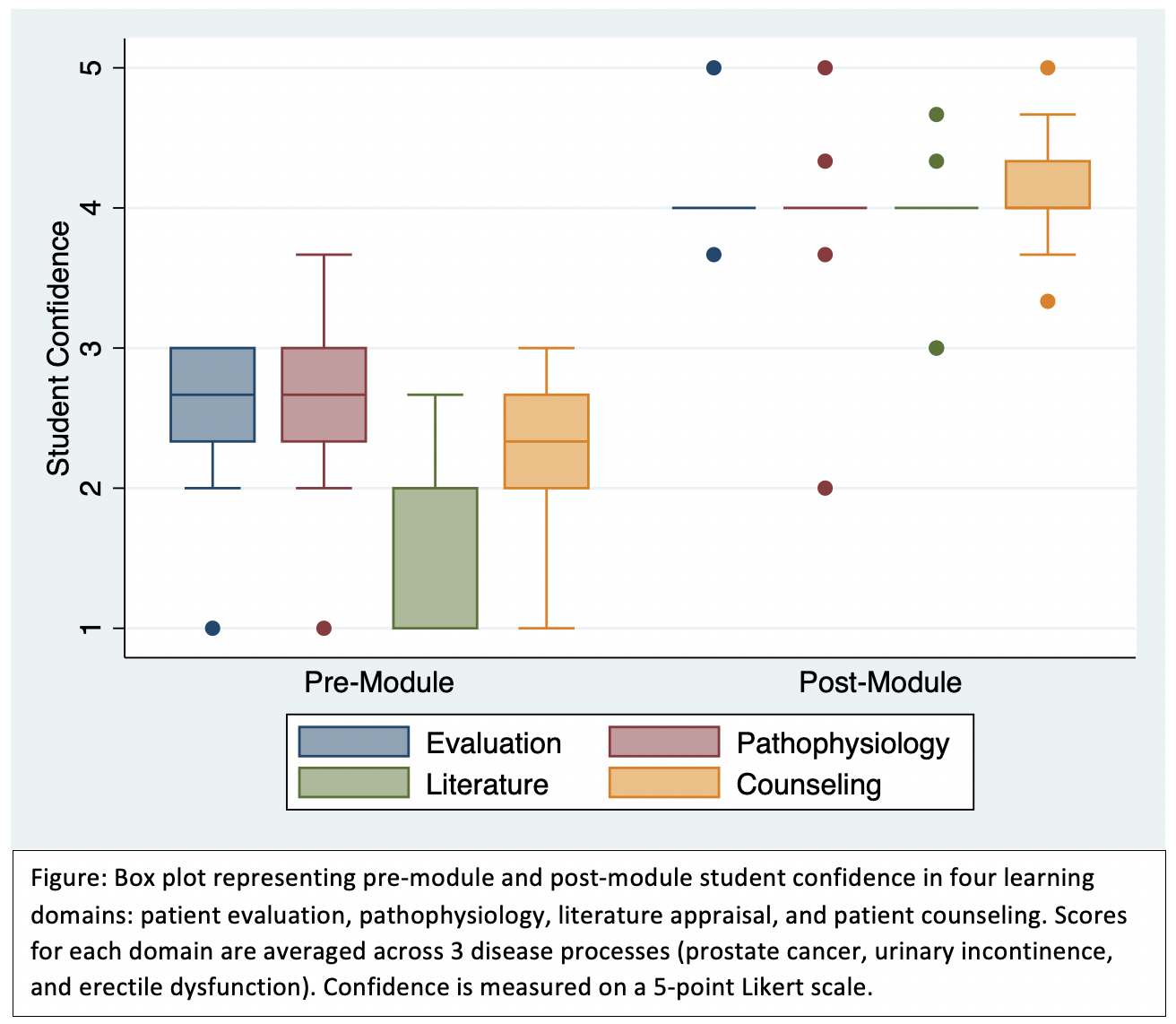
Methods: We created an online case-based urology module using the Canvas platform (Instructure, Salt Lake City, UT) with sections on prostate cancer, urinary incontinence, and erectile dysfunction. In August-September 2021, 21 students at 4 institutions completed the module as a component of their urology elective. Students answered questions on a discussion board and engaged in asynchronous dialogue with physicians at their institution. Students completed anonymous pre-module and post-module surveys assessing their confidence in 4 domains of learning for each disease process: patient evaluation, pathophysiology, literature appraisal, and patient counseling. Outcomes in each domain were scored on a 5-point Likert scale, and scores were averaged across the 3 disease processes (prostate cancer, urinary incontinence, and erectile dysfunction). Outcomes were compared using Wilcoxon signed-rank tests.
Results: Nine students (43% response rate) completed both the pre-module and post-module surveys. Median confidence scores increased across all 4 learning domains (Figure): patient evaluation (4.0 vs. 2.7, p=0.007), pathophysiology (4.0 vs. 2.7, p=0.007), literature appraisal (4.0 vs. 2.0, p=0.007), and patient counseling (4.0 vs. 2.3, p=0.008). Overall, 7/9 students rated the module “excellent” or “very good.” At least 7/9 students “strongly agree” or “somewhat agree” that the module was effective in learning foundational knowledge, improving critical thinking, facilitating performance assessment, and facilitating individualized feedback from the instructors; 6/9 students felt that online modules should be incorporated into future urology electives.
Conclusions: In a multi-institutional pilot, an interactive online curriculum for medical students improved confidence across learning domains for multiple disease processes. We plan to expand this program to more institutions and additional disease processes in order to improve medical student urologic education.
Source of Funding: Society of Academic Urologists
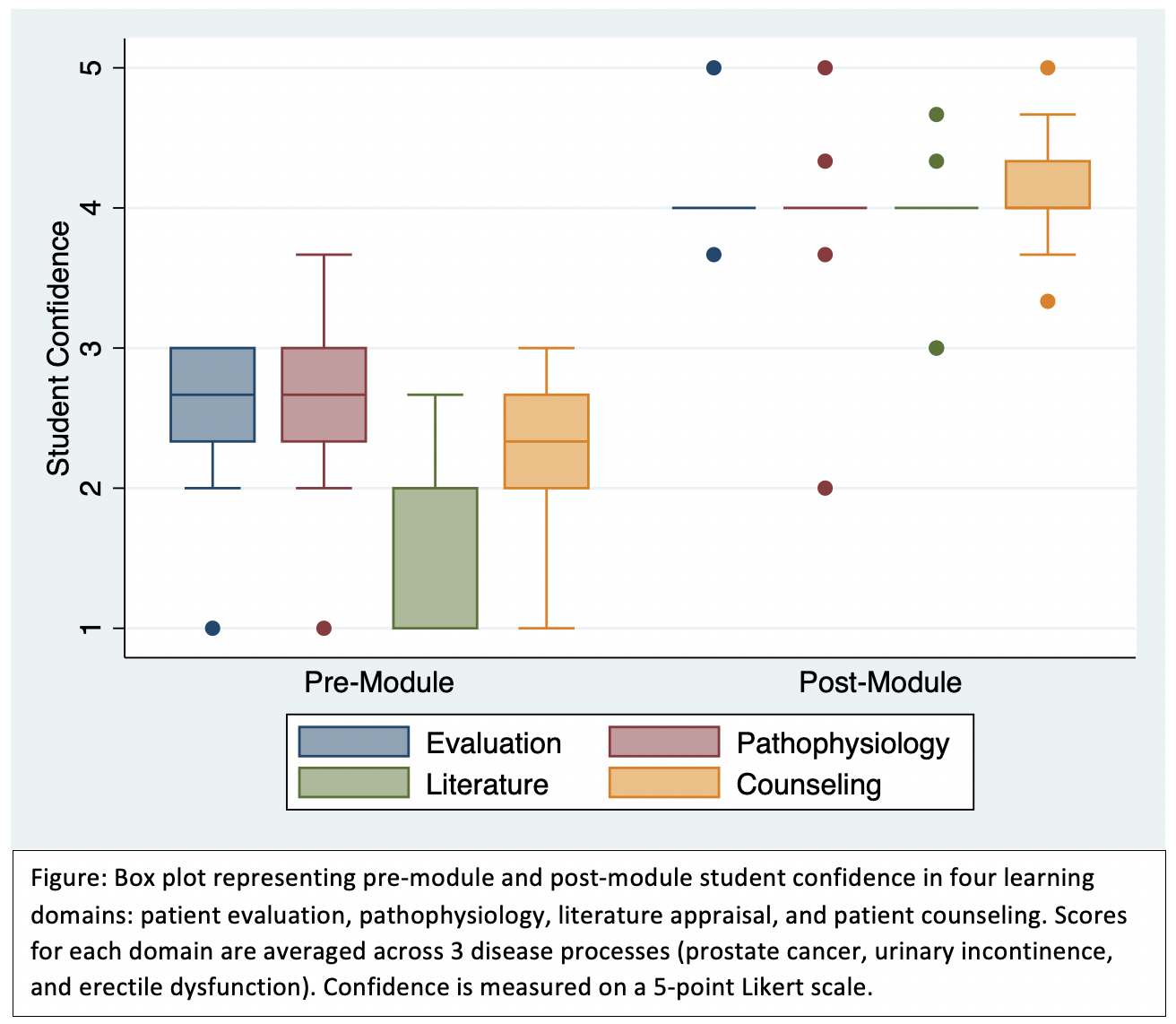
Methods: We created an online case-based urology module using the Canvas platform (Instructure, Salt Lake City, UT) with sections on prostate cancer, urinary incontinence, and erectile dysfunction. In August-September 2021, 21 students at 4 institutions completed the module as a component of their urology elective. Students answered questions on a discussion board and engaged in asynchronous dialogue with physicians at their institution. Students completed anonymous pre-module and post-module surveys assessing their confidence in 4 domains of learning for each disease process: patient evaluation, pathophysiology, literature appraisal, and patient counseling. Outcomes in each domain were scored on a 5-point Likert scale, and scores were averaged across the 3 disease processes (prostate cancer, urinary incontinence, and erectile dysfunction). Outcomes were compared using Wilcoxon signed-rank tests.
Results: Nine students (43% response rate) completed both the pre-module and post-module surveys. Median confidence scores increased across all 4 learning domains (Figure): patient evaluation (4.0 vs. 2.7, p=0.007), pathophysiology (4.0 vs. 2.7, p=0.007), literature appraisal (4.0 vs. 2.0, p=0.007), and patient counseling (4.0 vs. 2.3, p=0.008). Overall, 7/9 students rated the module “excellent” or “very good.” At least 7/9 students “strongly agree” or “somewhat agree” that the module was effective in learning foundational knowledge, improving critical thinking, facilitating performance assessment, and facilitating individualized feedback from the instructors; 6/9 students felt that online modules should be incorporated into future urology electives.
Conclusions: In a multi-institutional pilot, an interactive online curriculum for medical students improved confidence across learning domains for multiple disease processes. We plan to expand this program to more institutions and additional disease processes in order to improve medical student urologic education.
Source of Funding: Society of Academic Urologists

.jpg)
.jpg)