Back
Poster, Podium & Video Sessions
Moderated Poster
MP11: Pediatric Urology: Neurogenic Bladder, Reconstruction & Urologic Emergencies
MP11-13: Short and Long Term Renal Outcomes in Clinically Matched Cohorts of Newborns with PUV Managed by Primary Vesicostomy Versus Primary Valve Ablation
Friday, May 13, 2022
1:00 PM – 2:15 PM
Location: Room 225
Nora Haney*, Shwetha Mudalegundi, Angelica Griggs-Demmin, Tamir Sholklapper, Edwin Smith, Charlotte Wu, Baltimore, MD

Nora M. Haney, MD, MBA
Johns Hopkins Hospital
Poster Presenter(s)
Introduction: Some controversy exists regarding whether primary valve ablation (PVA) or primary vesicostomy (PVES) provides superior drainage in neonates with posterior urethral valves. We previously demonstrated progressive urethral dilation (PUD) as a means to achieve PVA in low birth weight and early gestational age neonates, who otherwise disproportionately require PVES. Management with PUD has provided a novel opportunity for comparative analysis of primary intervention on outcomes between similar cohorts with fewer clinical confounders. In this multi-institutional study, our objectives were to determine the short and long term renal outcomes in clinically matched cohorts of neonates with PVES versus PVA.
Methods: This is a retrospective study. Institution A performs PUD to achieve PVA in all neonates. Institution B performs PVES when PVA is unfeasible. Patients were matched primarily by creatinine at intervention and then by clinical features of gestational age, age at ablation, and weight at ablation. We excluded children who had intervention beyond 9 months of age or with incomplete creatinine data. We included all patients who met criteria over 25 years of follow up.
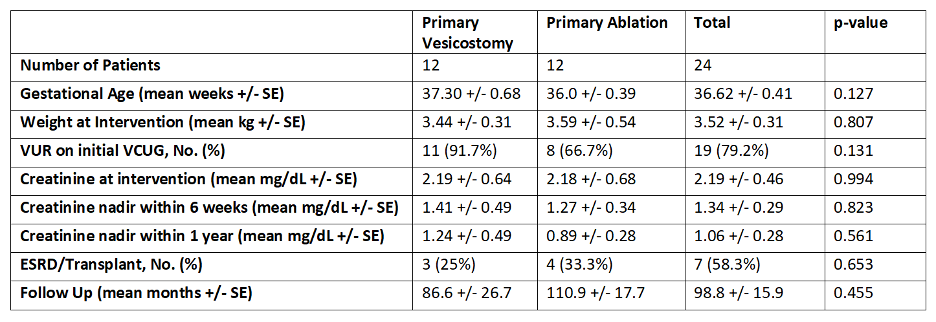
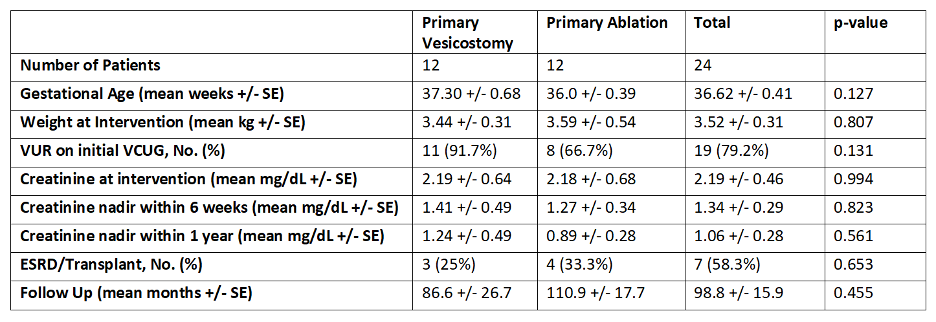
Results: 24 patients (12 PVES, 12 PVA) were included with mean follow up 98.8 (+/- 15.9) months. Clinical demographics were matched similarly between groups (Table 1). Creatinine nadir within 6 weeks and 1 year of intervention was not statistically significantly different between groups at 1.4 and 1.2 mg/dL respectively for PVES and 1.3 and 0.9 mg/dL respectively for PVA. A time to event analysis with Mantel-Cox Log Rank was performed and did not show a statistically significant difference in the long-term distribution of ESRD outcomes over time, p=0.819).
Conclusions: In these clinically matched cohorts comparing PVA to PVES, there was no statistically significant difference in renal outcomes in the short term as determined by creatinine nadir within 6 weeks and 1 year of primary intervention. Long-term results similarly show no statistically significant difference in ESRD outcomes. Although these are preliminary findings based on a small sample, this is the first study of this kind to provide insight into the effect of primary intervention on renal outcomes while reducing critical biases of inherently heterogeneous cohorts.
Source of Funding: None
Methods: This is a retrospective study. Institution A performs PUD to achieve PVA in all neonates. Institution B performs PVES when PVA is unfeasible. Patients were matched primarily by creatinine at intervention and then by clinical features of gestational age, age at ablation, and weight at ablation. We excluded children who had intervention beyond 9 months of age or with incomplete creatinine data. We included all patients who met criteria over 25 years of follow up.
Results: 24 patients (12 PVES, 12 PVA) were included with mean follow up 98.8 (+/- 15.9) months. Clinical demographics were matched similarly between groups (Table 1). Creatinine nadir within 6 weeks and 1 year of intervention was not statistically significantly different between groups at 1.4 and 1.2 mg/dL respectively for PVES and 1.3 and 0.9 mg/dL respectively for PVA. A time to event analysis with Mantel-Cox Log Rank was performed and did not show a statistically significant difference in the long-term distribution of ESRD outcomes over time, p=0.819).
Conclusions: In these clinically matched cohorts comparing PVA to PVES, there was no statistically significant difference in renal outcomes in the short term as determined by creatinine nadir within 6 weeks and 1 year of primary intervention. Long-term results similarly show no statistically significant difference in ESRD outcomes. Although these are preliminary findings based on a small sample, this is the first study of this kind to provide insight into the effect of primary intervention on renal outcomes while reducing critical biases of inherently heterogeneous cohorts.
Source of Funding: None

.jpg)
.jpg)