Back
Poster, Podium & Video Sessions
Moderated Poster
MP12: Kidney Cancer: Advanced (including Drug Therapy) I
MP12-04: Predictive impact of early changes in serum C-reactive protein levels in nivolumab plus ipilimumab therapy for metastatic renal cell carcinoma
Friday, May 13, 2022
1:00 PM – 2:15 PM
Location: Room 222
Hidekazu Tachibana*, Yuki Nemoto, Saitama, Japan, Hiroki Ishihara, Hironori Fukuda, Kazuhiko Yoshida, Junpei Iizuka, Tokyo, Japan, Yasunobu Hashimoto, Saitama, Japan, Tsunenori Kondo, Kazunari Tanabe, Toshio Takagi, Tokyo, Japan
- HT
Hidekazu Tachibana, MD, PHD
Saiseikai Kazo Hospital
Poster Presenter(s)
Introduction: Serum C-reactive protein (CRP) is reportedly associated with metastatic renal cell carcinoma (mRCC) activity. However, in the era of immune checkpoint inhibitors, the predictive value of CRP is unclear. In this study, we investigated the predictive impact of pretreatment CRP levels and early changes in CRP levels for the treatment of mRCC with nivolumab plus ipilimumab (NIVO-IPI) therapy.
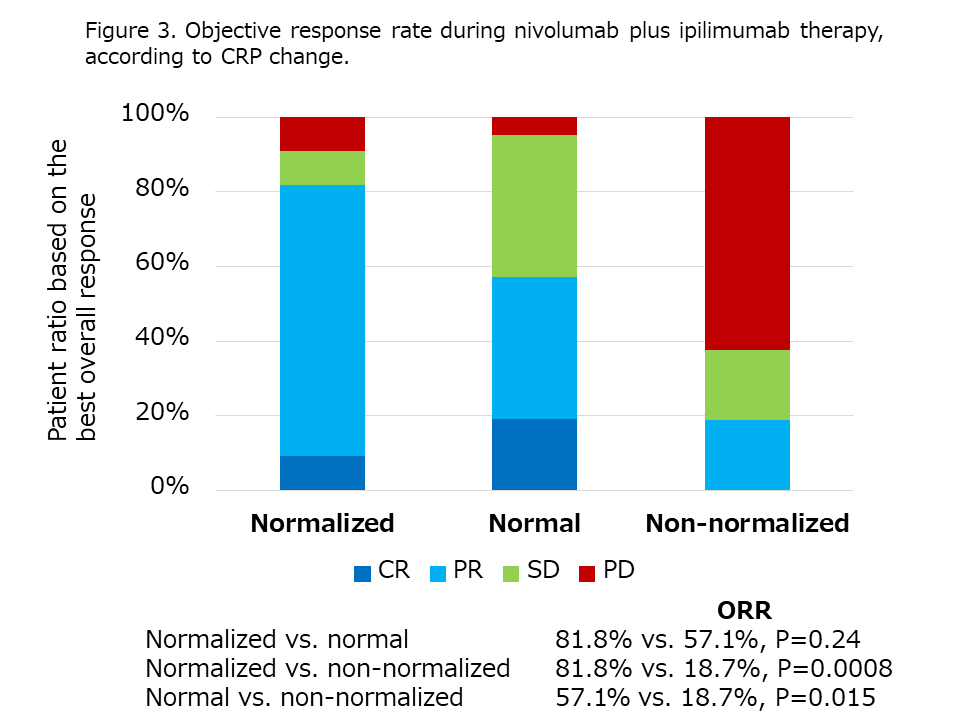
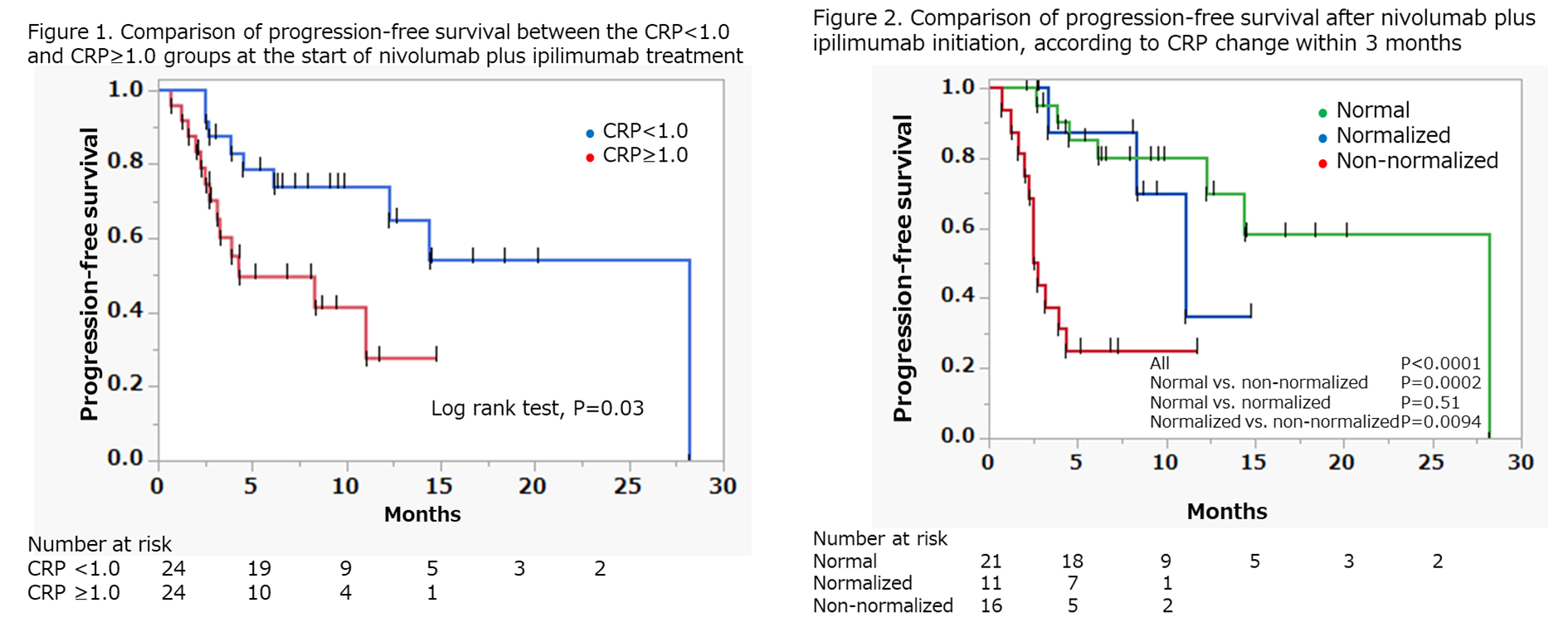
Methods: Forty-eight patients with mRCC treated with NIVO-IPI as a first-line therapy were retrospectively analyzed. First, patients were divided into 2 groups: initial CRP =1.0 mg/dL and <1.0 mg/dL. Progression-free survival (PFS) was compared between the 2 groups. Second, based on the CRP change within the first three months of NIVO-IPI, patients were placed in the normal group (CRP remains <1.0 mg/dL), normalized group (CRP decreased <1.0 mg/dL), and non-normalized group (CRP remained or increased to =1.0 mg/dL). The predictive association between CRP change and PFS was evaluated.
Results: PFS was significantly lower in the high initial CRP group (n=24, 50%) compared to the normal CRP group (n=24, 50%) (median: 4.3 vs. 28.1 months, P=0.03). As for the early CRP change, the normal (2.7 vs. 28.1, P=0.0002) and normalized (2.7 vs. 11.0, P=0.0094) groups showed significantly higher PFS, compared to the non-normalized group. Meanwhile, there was no significant difference between normal and normalized groups (P=0.51). The objective response rate was higher in the normal (57.1% vs. 18.7%, P=0.015) and normalized (81.8 vs. 18.7%, P=0.0008) groups, compared to the non-normalized group. Multivariate Cox regression analysis showed that normal [Hazard ratio (HR)=0.15, 95% Confidence interval (CI)=0.02-0.70, P=0.026] and normalized (HR 0.21, 95% CI=0.05-0.73, P=0.015) CRP showed significant association with PFS.
Conclusions: In the NIVO-IPI therapy for mRCC, early changes in CRP could predict PFS. This data may be useful for the early detection of ineffective NIVO-IPI therapy and conversion to subsequent therapies
Source of Funding: none
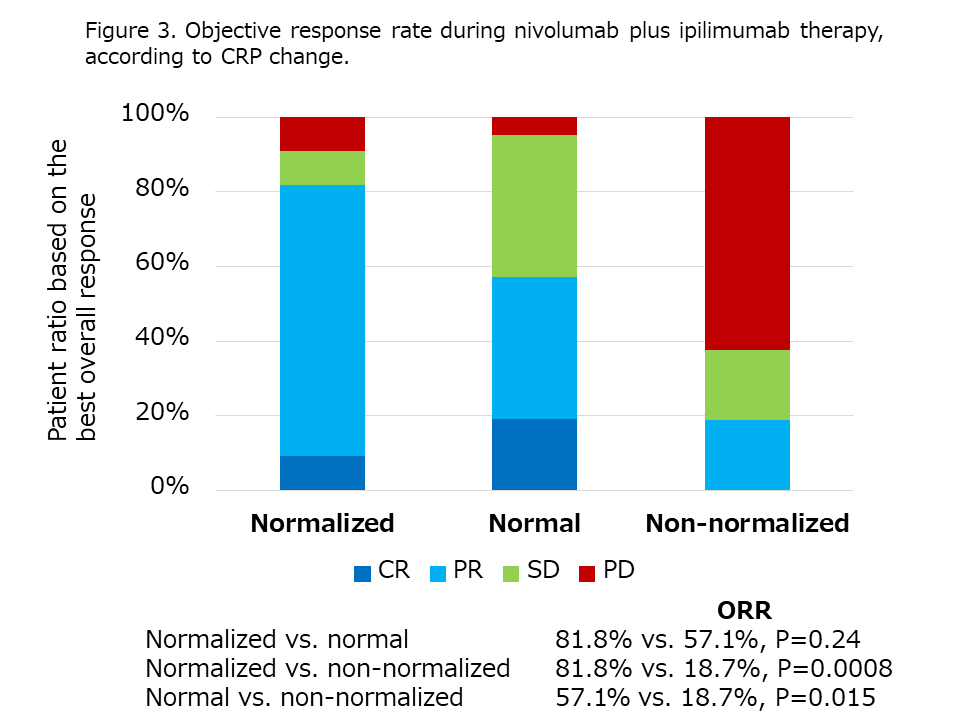
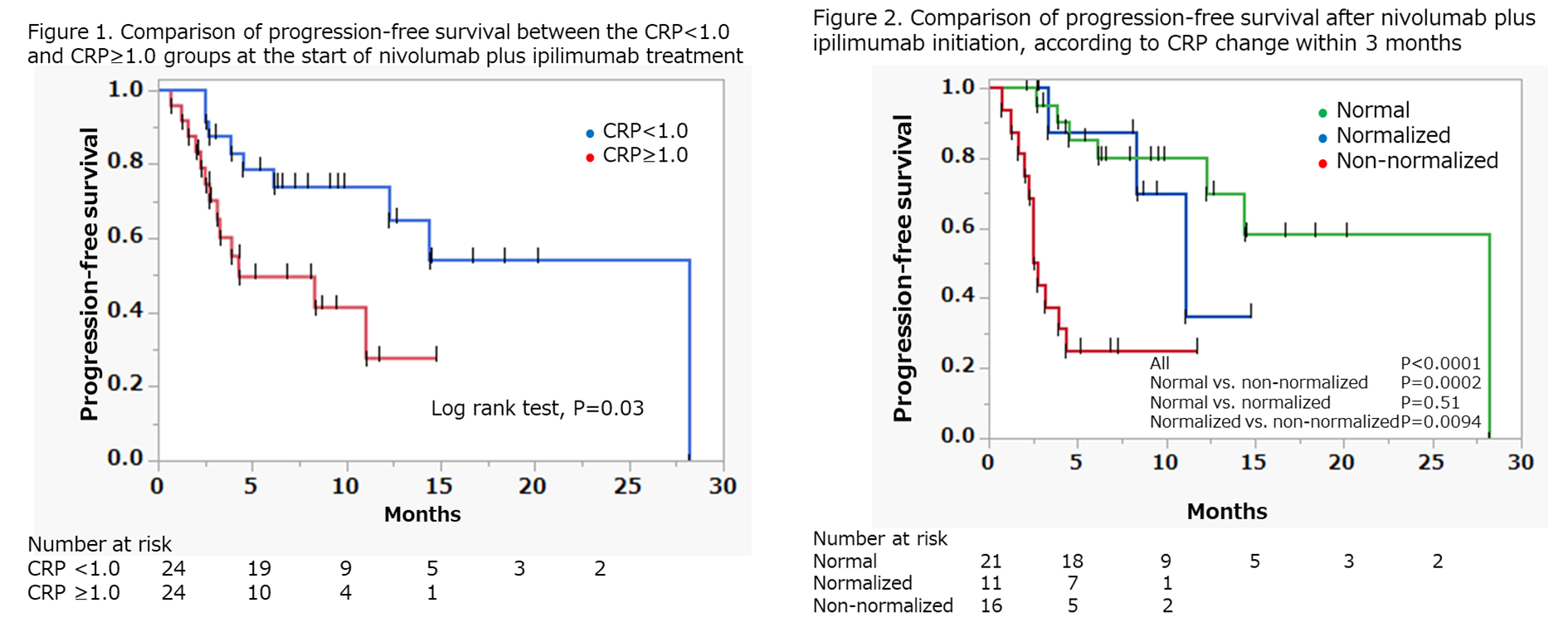
Methods: Forty-eight patients with mRCC treated with NIVO-IPI as a first-line therapy were retrospectively analyzed. First, patients were divided into 2 groups: initial CRP =1.0 mg/dL and <1.0 mg/dL. Progression-free survival (PFS) was compared between the 2 groups. Second, based on the CRP change within the first three months of NIVO-IPI, patients were placed in the normal group (CRP remains <1.0 mg/dL), normalized group (CRP decreased <1.0 mg/dL), and non-normalized group (CRP remained or increased to =1.0 mg/dL). The predictive association between CRP change and PFS was evaluated.
Results: PFS was significantly lower in the high initial CRP group (n=24, 50%) compared to the normal CRP group (n=24, 50%) (median: 4.3 vs. 28.1 months, P=0.03). As for the early CRP change, the normal (2.7 vs. 28.1, P=0.0002) and normalized (2.7 vs. 11.0, P=0.0094) groups showed significantly higher PFS, compared to the non-normalized group. Meanwhile, there was no significant difference between normal and normalized groups (P=0.51). The objective response rate was higher in the normal (57.1% vs. 18.7%, P=0.015) and normalized (81.8 vs. 18.7%, P=0.0008) groups, compared to the non-normalized group. Multivariate Cox regression analysis showed that normal [Hazard ratio (HR)=0.15, 95% Confidence interval (CI)=0.02-0.70, P=0.026] and normalized (HR 0.21, 95% CI=0.05-0.73, P=0.015) CRP showed significant association with PFS.
Conclusions: In the NIVO-IPI therapy for mRCC, early changes in CRP could predict PFS. This data may be useful for the early detection of ineffective NIVO-IPI therapy and conversion to subsequent therapies
Source of Funding: none

.jpg)
.jpg)