Back
Poster, Podium & Video Sessions
Moderated Poster
MP12: Kidney Cancer: Advanced (including Drug Therapy) I
MP12-07: The anatomical location of lymphadenopathies at imaging predicts the risk of lymph node invasion at final pathology in patients with renal cell carcinoma
Friday, May 13, 2022
1:00 PM – 2:15 PM
Location: Room 222
Giuseppe Rosiello*, Giuseppe Fallara, Giuseppe Basile, Daniele Cignoli, Francesco De Cobelli, Giorgio Brembilla, Luigi Nocera, Federico Belladelli, Gianmarco Colandrea, Daniela Canibus, Giacomo Musso, Francesco Cei, Chiara Re, Cristina Giancristofaro, Alberto Briganti, Roberto Bertini, Andrea Necchi, Daniele Raggi, Milan, Italy, Alexandre Mottrie, Aalst, Belgium, Pierre I. Karakiewicz, Montreal, Canada, Francesco Montorsi, Andrea Salonia, Alessandro Larcher, Umberto Capitanio, Milan, Italy

Giuseppe Rosiello, MD
Resident
San Raffaele Hospital
Poster Presenter(s)
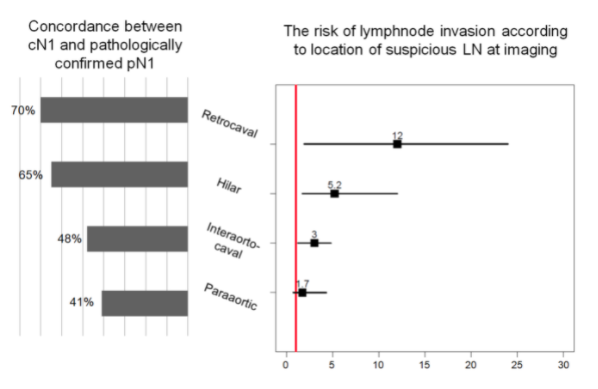
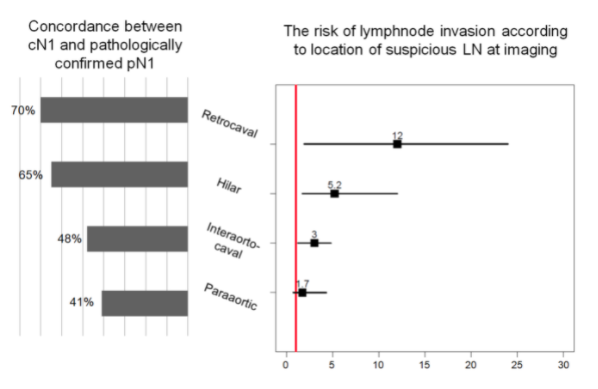
Introduction: The positive predictive value of preoperative imaging in detecting pathologically confirmed lymph node invasion (LNI) in patients with renal cell carcinoma (RCC) ranges from 33 to 56%. The aim of the study was to evaluate the risk of LNI according to the location of suspicious LN at preoperative imaging, to better identifying those patients in whom lymph node dissection (LND) may be indicated.
Methods: Within a prospectively maintained database, we identified 1,048 patients treated with surgery for RCC at a single tertiary centre between 2000 and 2021. Lymphadenopathy was defined a suspicious lymph node with axial diameter >1 cm. Location of lymphadenopathy was categorized as follows: 1) hilar; 2) interaortocaval; 3) paraortic; 4) retrocaval. Separate multivariable logistic regression analyses were performed to assess the risk of LNI for each anatomical location.
Results: Out of 1,048 patients, 192 (18%) patients had at least one lymphadenopathy at preoperative imaging. Median age at surgery was 61 [Interquartile range (IQR): 51 - 70] years and median tumor size was 7 (IQR: 5-9) cm. Median number of LN removed was 5 (IQR: 3-10). LNI location at axial imaging resulted as follows: 67% paraortic; 35% interaortocaval; 27% hilar; 16% retrocaval. In a per-region analysis, the concordance rate according to suspicious LN metastasis’s location was 41 vs. 48 vs. 65 vs. 70% for paraortic vs. interaortocaval vs. hilar vs. retrocaval, respectively. At multivariable analyses, the risk of pathologically confirmed LNI varied according to suspicious LN location (Figure 1).
Conclusions: The concordance between clinical and pathologically LNI in RCC significantly varies according to the anatomical location. Hilar and retrocaval suspicious lymphadenopathies are associated with higher concordance and increased risk of LNI. In consequence, performing a more extended LND for staging purposes in these patients may allow for a better risk classification and for a better planning of adjuvant treatments.
Source of Funding: no
Methods: Within a prospectively maintained database, we identified 1,048 patients treated with surgery for RCC at a single tertiary centre between 2000 and 2021. Lymphadenopathy was defined a suspicious lymph node with axial diameter >1 cm. Location of lymphadenopathy was categorized as follows: 1) hilar; 2) interaortocaval; 3) paraortic; 4) retrocaval. Separate multivariable logistic regression analyses were performed to assess the risk of LNI for each anatomical location.
Results: Out of 1,048 patients, 192 (18%) patients had at least one lymphadenopathy at preoperative imaging. Median age at surgery was 61 [Interquartile range (IQR): 51 - 70] years and median tumor size was 7 (IQR: 5-9) cm. Median number of LN removed was 5 (IQR: 3-10). LNI location at axial imaging resulted as follows: 67% paraortic; 35% interaortocaval; 27% hilar; 16% retrocaval. In a per-region analysis, the concordance rate according to suspicious LN metastasis’s location was 41 vs. 48 vs. 65 vs. 70% for paraortic vs. interaortocaval vs. hilar vs. retrocaval, respectively. At multivariable analyses, the risk of pathologically confirmed LNI varied according to suspicious LN location (Figure 1).
Conclusions: The concordance between clinical and pathologically LNI in RCC significantly varies according to the anatomical location. Hilar and retrocaval suspicious lymphadenopathies are associated with higher concordance and increased risk of LNI. In consequence, performing a more extended LND for staging purposes in these patients may allow for a better risk classification and for a better planning of adjuvant treatments.
Source of Funding: no

.jpg)
.jpg)