Back
Poster, Podium & Video Sessions
Moderated Poster
MP12: Kidney Cancer: Advanced (including Drug Therapy) I
MP12-13: The role of nephrectomy in metastatic renal cell carcinoma in the era of immune-combination therapies: a meta-analysis
Friday, May 13, 2022
1:00 PM – 2:15 PM
Location: Room 222
Keiichiro Mori*, Fahad Quhal, Takafumi Yanagisawa, Satoshi Katayama, Benjamin Pradere, Ekaterina Laukhtina, Pawel Rajwa, Hadi Mostafaei, Reza Sari Motlagh, Vienna, Austria, Takahiro Kimura, Shin Egawa, Tokyo, Japan, Karim Bensalah, Rennes, France, Pierre Karakiewicz, Montreal, Canada, Manuela Schmidinger, Shahrokh Shariat, Vienna, Austria
Keiichiro Mori, MD, PhD
Medical University of Vienna
Poster Presenter(s)
Introduction: Recently, immune checkpoint inhibitor (ICI)-combination therapies have radically altered the treatment landscape in metastatic renal cell carcinoma (mRCC). No phase 3 trials have assessed the impact of cytoreductive nephrectomy (CN) for efficacy in mRCC patients treated with ICI-combination therapy. Thus, we assessed the role of CN in mRCC patients in the ICI-combination therapy era.
Methods: Multiple databases were searched for articles published until October 2021. Studies comparing overall survival (OS) and/or progression-free survival (PFS) in mRCC patients treated with ICI combination-therapy as first-line were deemed eligible.
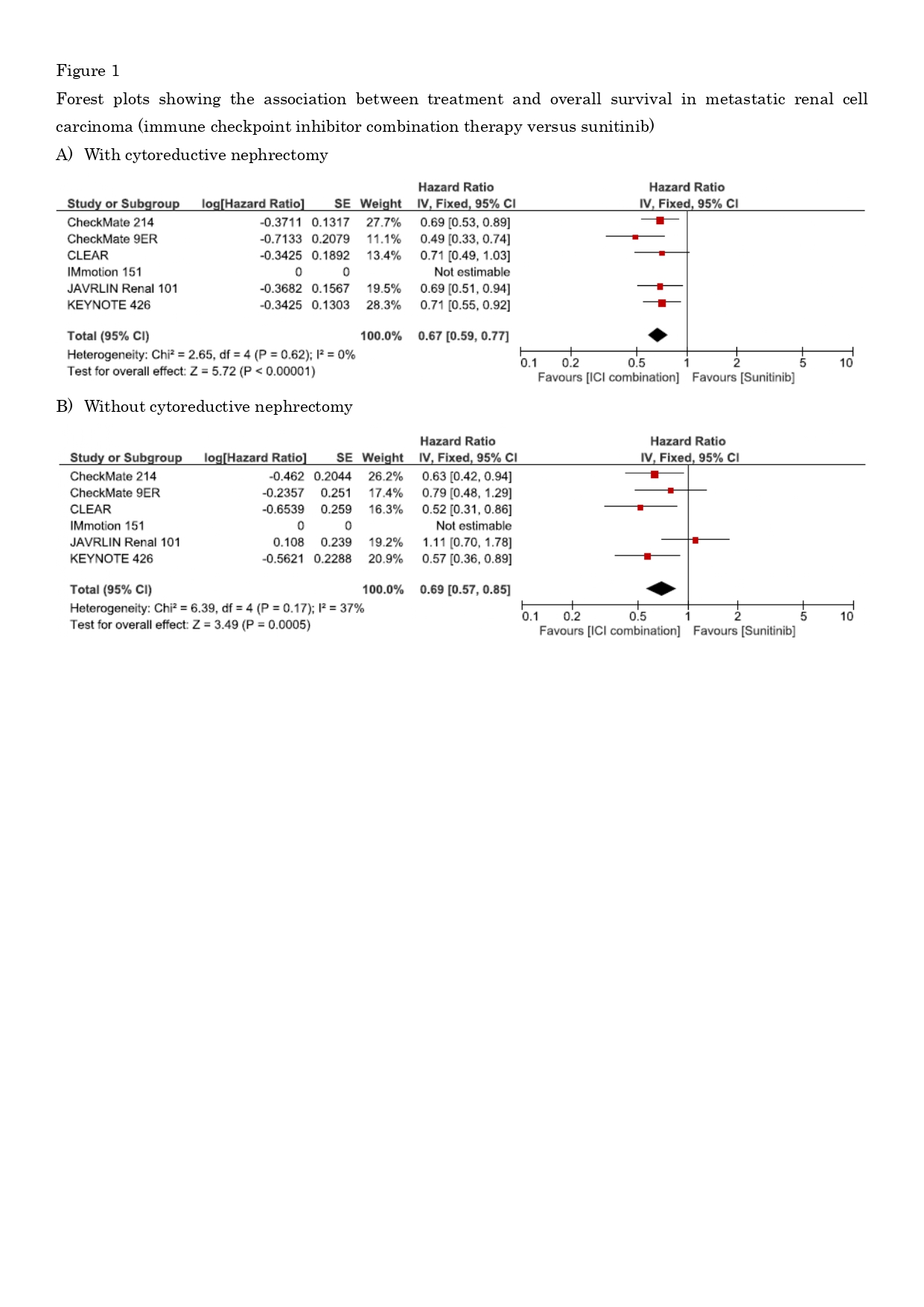
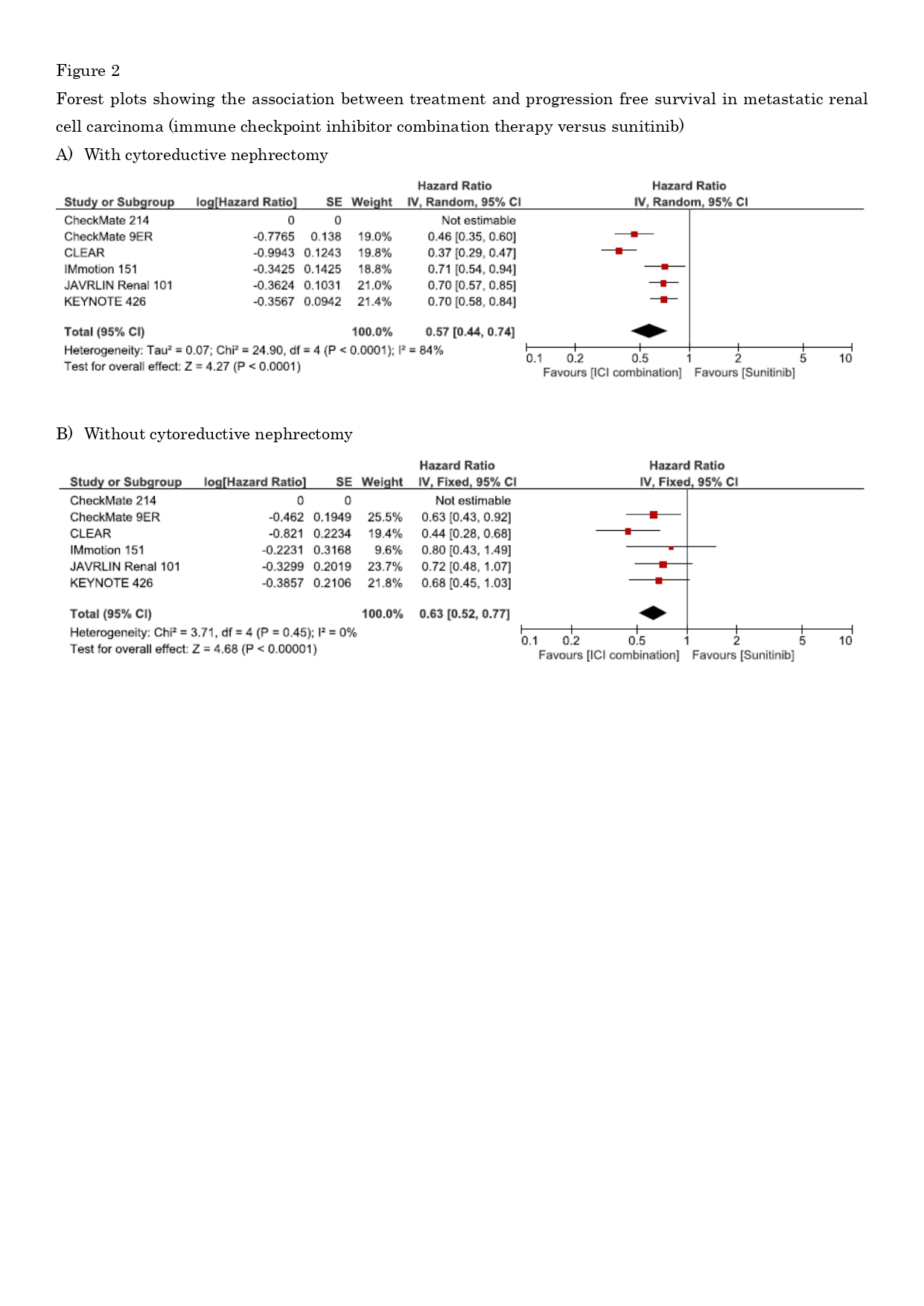
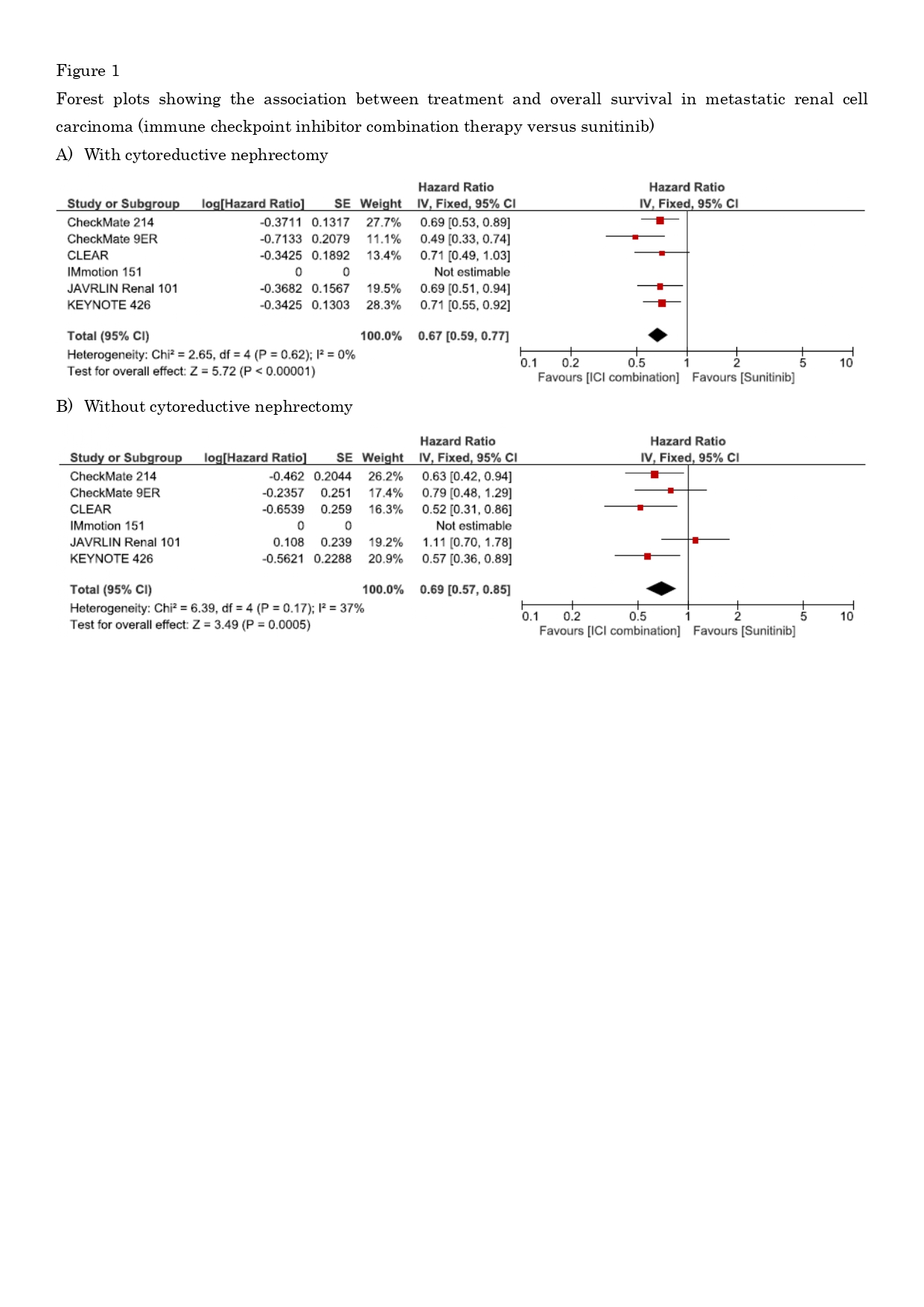
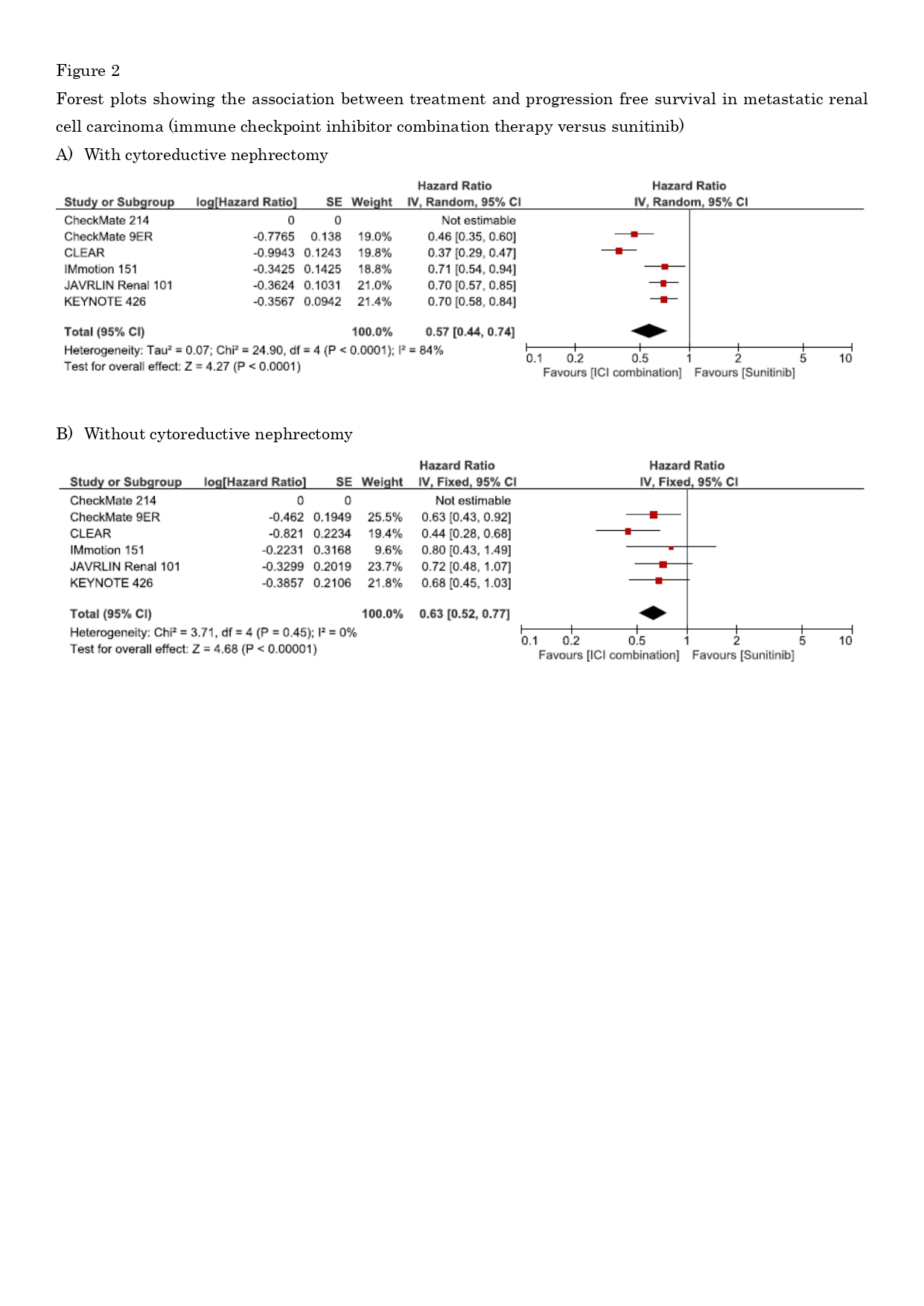
Results: Six studies met the eligibility criteria. ICI-combination therapy was associated with significantly better OS/PFS than sunitinib in patients who had undergone CN (hazard ratio [HR], 0.67; 95% confidence interval [CI], 0.59–0.77/HR, 0.57; 95% CI, 0.44–0.74, respectively; both P<0.001), and in those who had not (HR, 0.69; 95% CI, 0.57–0.85/ HR, 0.63; 95% CI, 0.52–0.77, respectively; both P<0.001). Although the OS and PFS benefits of ICI-combination therapy were larger in those undergoing CN, the HR for OS and PFS indicated that ICI-combination therapy’s treatment effect did not differ substantially with or without CN. In network meta-analyses, nivolumab plus cabozantinib was the most effective regimen in those undergoing CN, and pembrolizumab plus lenvatinib for those not undergoing CN.
Conclusions: CN offers limited survival benefits to mRCC patients receiving ICI-combination therapy. Careful patient selection remains paramount. As each ICI-combination regimen varied widely in its effect in those who had and had not undergone CN, CN may contribute to better treatment decision-making for ICI combination therapy recipients.
Source of Funding: No funding.
Methods: Multiple databases were searched for articles published until October 2021. Studies comparing overall survival (OS) and/or progression-free survival (PFS) in mRCC patients treated with ICI combination-therapy as first-line were deemed eligible.
Results: Six studies met the eligibility criteria. ICI-combination therapy was associated with significantly better OS/PFS than sunitinib in patients who had undergone CN (hazard ratio [HR], 0.67; 95% confidence interval [CI], 0.59–0.77/HR, 0.57; 95% CI, 0.44–0.74, respectively; both P<0.001), and in those who had not (HR, 0.69; 95% CI, 0.57–0.85/ HR, 0.63; 95% CI, 0.52–0.77, respectively; both P<0.001). Although the OS and PFS benefits of ICI-combination therapy were larger in those undergoing CN, the HR for OS and PFS indicated that ICI-combination therapy’s treatment effect did not differ substantially with or without CN. In network meta-analyses, nivolumab plus cabozantinib was the most effective regimen in those undergoing CN, and pembrolizumab plus lenvatinib for those not undergoing CN.
Conclusions: CN offers limited survival benefits to mRCC patients receiving ICI-combination therapy. Careful patient selection remains paramount. As each ICI-combination regimen varied widely in its effect in those who had and had not undergone CN, CN may contribute to better treatment decision-making for ICI combination therapy recipients.
Source of Funding: No funding.

.jpg)
.jpg)