Back
Poster, Podium & Video Sessions
Moderated Poster
MP13: Health Services Research: Practice Patterns, Quality of Life and Shared Decision Making I
MP13-01: Patient Perspectives in Genital Gender-Affirming Surgery: The Need for Patient Reported Outcome Measures
Friday, May 13, 2022
2:45 PM – 4:00 PM
Location: Room 228
Nnenaya Agochukwu-Mmonu, Elijah Castle*, Lee Zhao, Asa Radix, Rachel Bluebond-Langner, Daphna Harel, Danil Makarov, New York, NY, Clarissa Ospina-Norvell, San Francisco, CA, Carolyn Berry, New York, NY

Elijah Castle, BA
NYU Langone Health
Poster Presenter(s)
Introduction: To date, there has been no systematic evaluation of perspectives for transgender populations undergoing genital gender-affirming surgery (GGAS)–vaginoplasty, phalloplasty, and metoidioplasty–nor are there validated patient reported outcome measures (PROMs). PROMs elicit unfiltered patient feedback and empower patient-centered care. The scarcity of GGAS PROMs may negatively impact shared decision-making, which may adversely impact outcomes. The objective of this study is to elicit perspectives of transgender patients undergoing GGAS through a community based participatory research approach.
Methods: We recruited transgender patients undergoing GGAS from January-May 2021 for participation in virtual focus groups in partnership with LGBTQ community health centers (Table 1). We used guides developed with the patient community and qualitative research experts to lead discussions, focusing on patient experiences and expectations. Discussions were transcribed, coded, and analyzed using inductive and deductive coding to identify common themes, focusing on quotations coded with decision-making and/or patient-surgeon relationship.
Results: We held 9 total focus groups, with 3-6 participants per group (Table 1).
Qualitative analysis revealed divergent outcome expectations between patients and surgeons and not all patient goals were met. For example, one participant stated, “I would’ve been very uncomfortable telling my doctors that I didn’t want a vaginectomy— I didn’t want to seem like I was not fitting into what they expected.” Another participant expressed, “When I tried to ask about a revision, my surgeon said, ‘you don’t need it.'" A participant also reported experiencing “neglect and dismissiveness” when informing their surgeon something was wrong.
Conclusions: There currently exists disparity regarding defining successful and realistic outcomes between patients and surgeons; PROMs are critical to help facilitate these discussions. While physician outcome reporting is often prioritized, it is subject to bias and does not capture patient perspectives. A PROM tool developed through a community based participatory model may resolve these challenges.
Source of Funding: The project described was supported by the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health, through Grant Award Number 2KL2TR001446-06A1. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
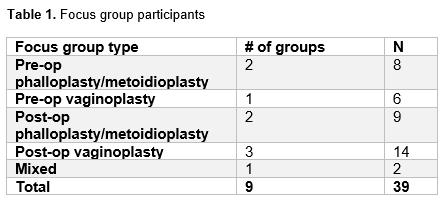
Methods: We recruited transgender patients undergoing GGAS from January-May 2021 for participation in virtual focus groups in partnership with LGBTQ community health centers (Table 1). We used guides developed with the patient community and qualitative research experts to lead discussions, focusing on patient experiences and expectations. Discussions were transcribed, coded, and analyzed using inductive and deductive coding to identify common themes, focusing on quotations coded with decision-making and/or patient-surgeon relationship.
Results: We held 9 total focus groups, with 3-6 participants per group (Table 1).
Qualitative analysis revealed divergent outcome expectations between patients and surgeons and not all patient goals were met. For example, one participant stated, “I would’ve been very uncomfortable telling my doctors that I didn’t want a vaginectomy— I didn’t want to seem like I was not fitting into what they expected.” Another participant expressed, “When I tried to ask about a revision, my surgeon said, ‘you don’t need it.'" A participant also reported experiencing “neglect and dismissiveness” when informing their surgeon something was wrong.
Conclusions: There currently exists disparity regarding defining successful and realistic outcomes between patients and surgeons; PROMs are critical to help facilitate these discussions. While physician outcome reporting is often prioritized, it is subject to bias and does not capture patient perspectives. A PROM tool developed through a community based participatory model may resolve these challenges.
Source of Funding: The project described was supported by the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health, through Grant Award Number 2KL2TR001446-06A1. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.

.jpg)
.jpg)