Back
Poster, Podium & Video Sessions
Moderated Poster
MP13: Health Services Research: Practice Patterns, Quality of Life and Shared Decision Making I
MP13-18: Impact of Comprehensive Health Insurance Coverage on Quality of Life in Low-Income Men with Prostate Cancer
Friday, May 13, 2022
2:45 PM – 4:00 PM
Location: Room 228
Allen E. D. Siapno*, Thomas W. Gaither, Megha D. Tandel, Lorna Kwan, Ying-Ying Meng, Sally Maliski, Arlene Fink, Mark S. Litwin, Los Angeles, CA

Allen Enrique Siapno
Medical Student
Charles R. Drew University/David Geffen School of Medicine, UCLA
Poster Presenter(s)
Introduction: The Affordable Care Act (ACA) expanded Medicaid coverage to a portion of previously uninsured low-income men receiving free disease-focused navigation-based care through the Improving Access, Counseling and Treatment for Californians with Prostate Cancer (IMPACT) program. To determine the effect of the transition to comprehensive health insurance on health-related quality of life (QoL), we compared men who transitioned to full-scope insurance through the ACA to men who were ACA-ineligible and continued care in IMPACT.
Methods: We retrospectively reviewed survey data on IMPACT enrollees when the ACA went into effect in 2014, creating a natural experimental cohort with some men transitioning from IMPACT to ACA coverage (intervention group) and other men remaining in IMPACT (control group). Subjects completed three surveys: one year before, at, and one year after the transition. The main outcomes were two composite domains of general QoL in the RAND 12-Item Health Survey (SF-12) and six domains of prostate cancer-specific QoL in the UCLA Prostate Cancer Index. Statistical analysis compared demographics, clinical characteristics, and the QoL measures. We assessed the independent effects of ACA coverage on QoL outcomes using repeated-measures regression.
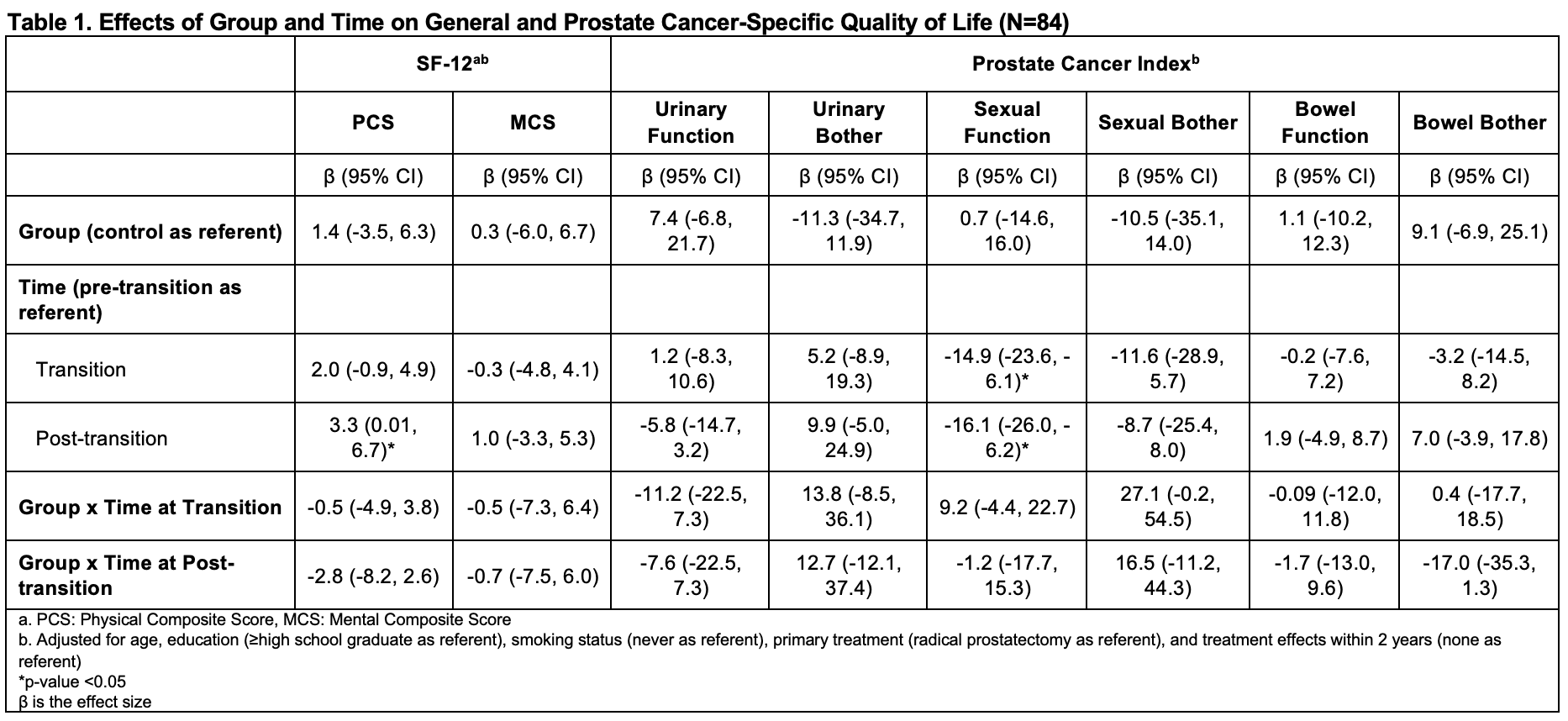
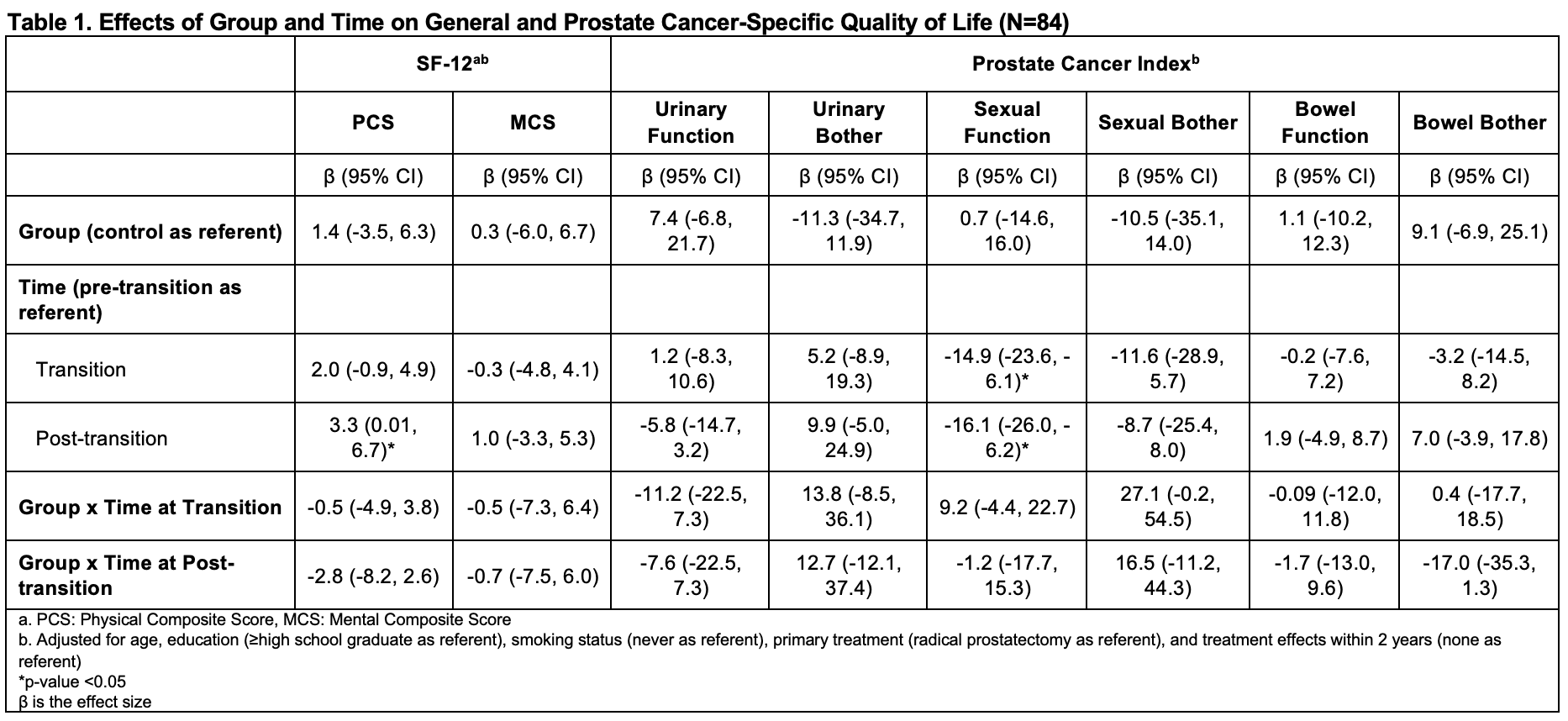
Results: 84 men (30 intervention, 54 control) met inclusion criteria. Mean age was 61.3 years (SD 7.4), 82% were Hispanic, and 64% were living with their spouse/partner. At the transition, the intervention group was enrolled in IMPACT for less time (40% vs 70% enrolled >1 year, p=0.02) and were less likely to be actively smoking (30% vs 54%, p=0.04). QoL scores at the transition were similar for both groups except for better sexual function in the intervention group (40.0 vs 23.7, p=0.01). QoL did not differ over time between the groups, but sexual function in both groups declined from pre- to post-transition (Table 1).
Conclusions: Both of those who transitioned to full-scope insurance or remained in a free prostate cancer treatment program had stable general and prostate cancer-specific QoL. Decline in sexual function may be time- or age-related. High-touch navigation aspects of a disease-focused program may have contributed to stability in outcomes.
Source of Funding: IMPACT receives funding from the California Department of Health Care Services. Research was funded by the American Cancer Society Research Grant.
Methods: We retrospectively reviewed survey data on IMPACT enrollees when the ACA went into effect in 2014, creating a natural experimental cohort with some men transitioning from IMPACT to ACA coverage (intervention group) and other men remaining in IMPACT (control group). Subjects completed three surveys: one year before, at, and one year after the transition. The main outcomes were two composite domains of general QoL in the RAND 12-Item Health Survey (SF-12) and six domains of prostate cancer-specific QoL in the UCLA Prostate Cancer Index. Statistical analysis compared demographics, clinical characteristics, and the QoL measures. We assessed the independent effects of ACA coverage on QoL outcomes using repeated-measures regression.
Results: 84 men (30 intervention, 54 control) met inclusion criteria. Mean age was 61.3 years (SD 7.4), 82% were Hispanic, and 64% were living with their spouse/partner. At the transition, the intervention group was enrolled in IMPACT for less time (40% vs 70% enrolled >1 year, p=0.02) and were less likely to be actively smoking (30% vs 54%, p=0.04). QoL scores at the transition were similar for both groups except for better sexual function in the intervention group (40.0 vs 23.7, p=0.01). QoL did not differ over time between the groups, but sexual function in both groups declined from pre- to post-transition (Table 1).
Conclusions: Both of those who transitioned to full-scope insurance or remained in a free prostate cancer treatment program had stable general and prostate cancer-specific QoL. Decline in sexual function may be time- or age-related. High-touch navigation aspects of a disease-focused program may have contributed to stability in outcomes.
Source of Funding: IMPACT receives funding from the California Department of Health Care Services. Research was funded by the American Cancer Society Research Grant.

.jpg)
.jpg)