Back
Poster, Podium & Video Sessions
Moderated Poster
MP14: Stone Disease: Surgical Therapy (including ESWL) I
MP14-11: Propensity Score-Matched Analysis Comparing Retrograde Intrarenal Surgery with Percutaneous Nephrolithotomy in Anomalous Kidneys
Friday, May 13, 2022
2:45 PM – 4:00 PM
Location: Room 225
Ee Jean Lim*, Singapore, Singapore, Jeremy Yuen-Chun Teoh, Hong Kong , China, People's Republic of, Khi Yung Fong, Singapore, Singapore, Esteban Emiliani, Barcelona , Spain, Nariman Gadzhiev, Dmitry Gorelov, Saint-Petersburg , Russian Federation, Yiloren Tanidir, Istanbul, Turkey, Fabio Sepulveda, San Paulo, Brazil, Abdullah Al-Terki, Kuwait, Kuwait, Sanjay Khadgi, Lalitpur, Nepal, Abhay Mahajan, Aurangabad, India, Deepak Ragoori, Banjara Hills, India, Govindarajan Ramalingam, Tamil Nadu, India, Vaddi Chandra Mohan, Hyderabad, India, Arvind Prakash Ganpule, Gujarat, India, Santosh Kumar, Vellore, India, Daniele Castellani, Ancona, Italy, Manoj Monga, California, CA, Scoffone Cesare, Turin, Italy, Fabio Vicentini, São Paulo, Brazil, Olivier Traxer, Paris, France, Bhaskar Kumar Somani, Southampton, United Kingdom, Vineet Gauhar, Singapore, Singapore
- EL
Poster Presenter(s)
Introduction: Endourologic interventions for urolithiasis in patients with anomalous kidneys can be challenging, and comparisons between these interventions are not well studied.
We aim to compare the safety, outcomes and complications of retrograde intrarenal surgery (RIRS) versus percutaneous nephrolithotomy (PCNL) in patients with urolithiasis in anomalous kidneys.
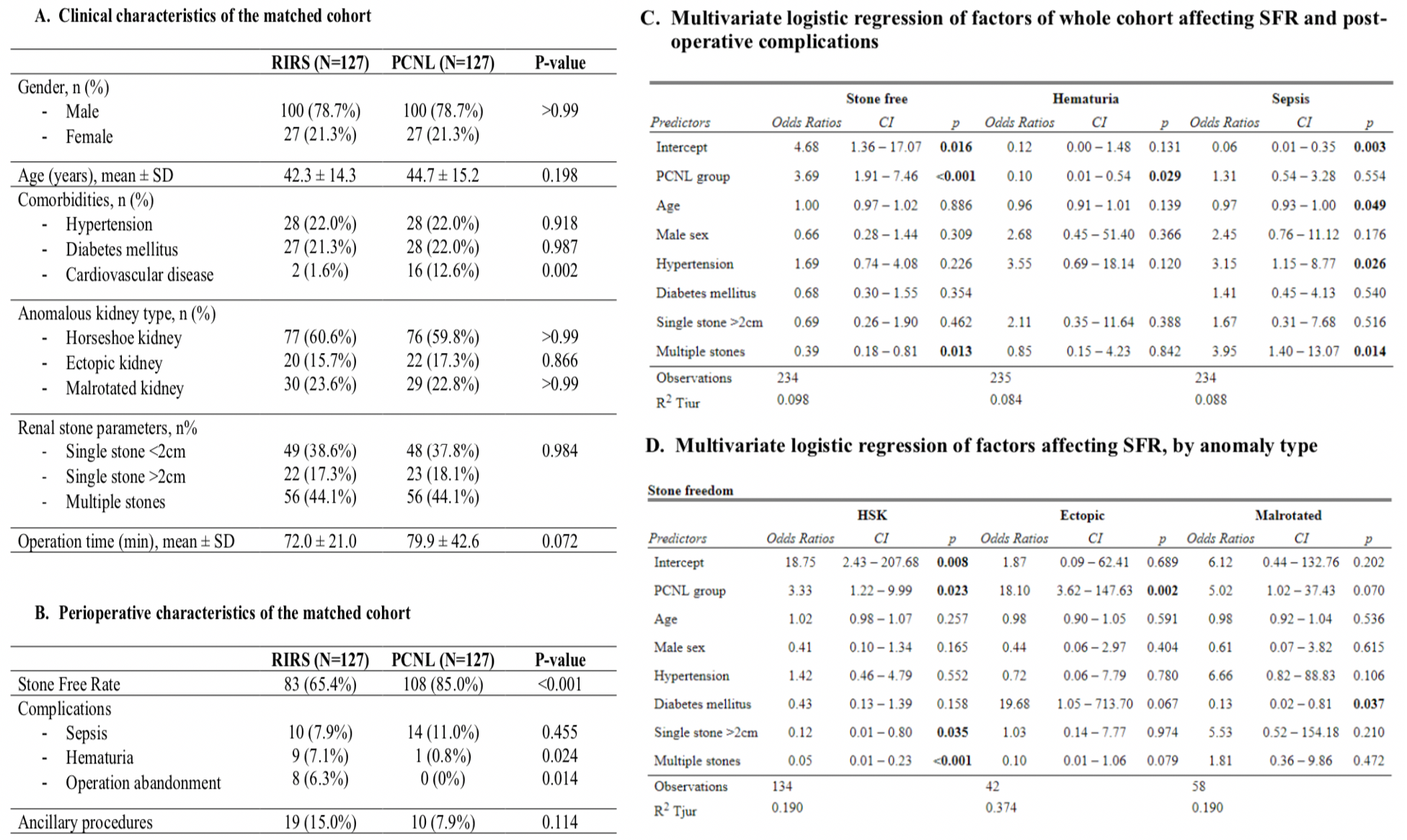
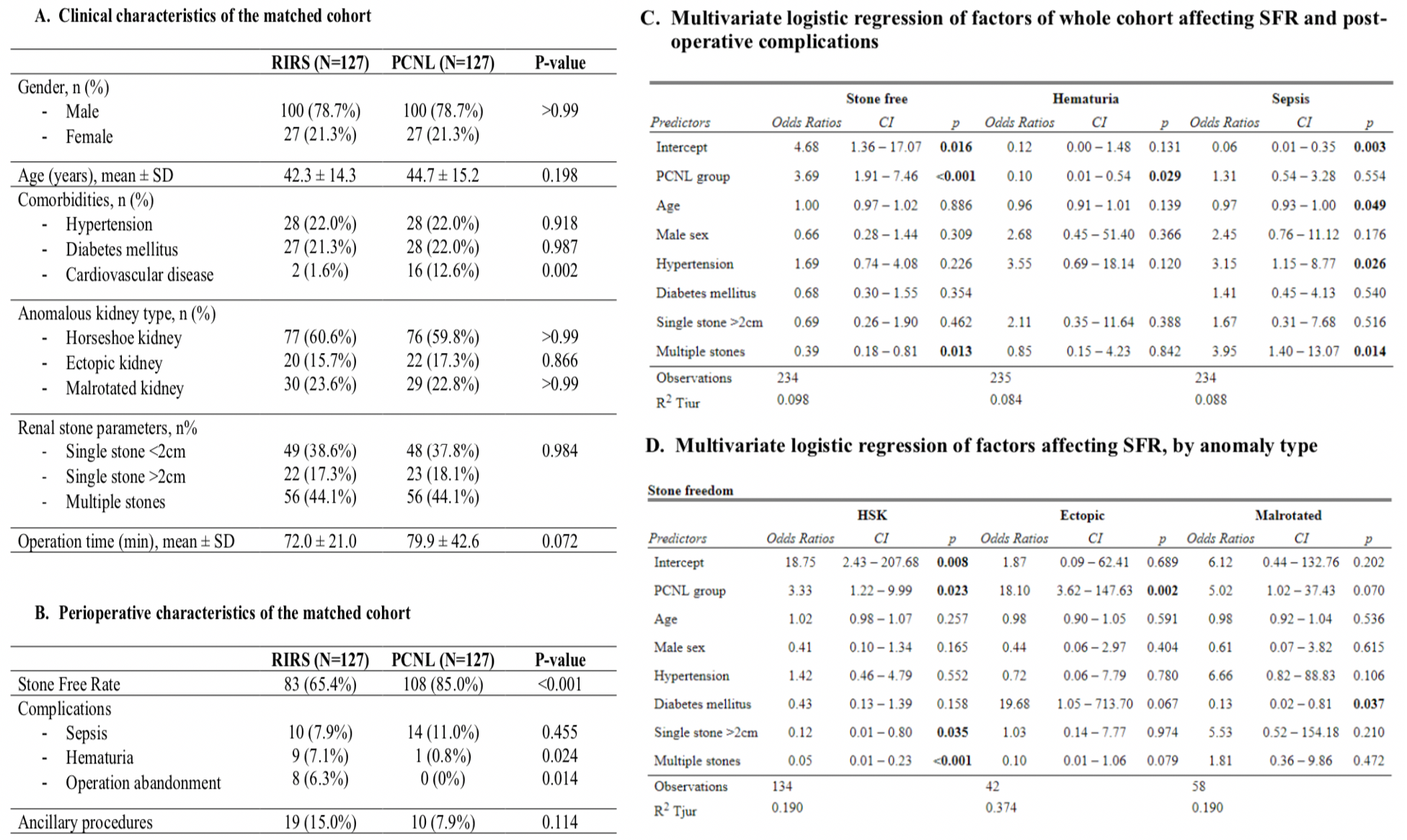
Methods: A propensity score-matched pair analysis (PSM) was performed on pooled patient data from 20 centers. 569 patients with anomalous kidneys (Horseshoe kidney(HSK), ectopic kidney, malrotated kidney) and urolithiasis who received either PCNL or RIRS as the primary modality of intervention from 2010 to 2020 were analyzed. Patients were matched based on calculated propensity scores by a regression model using age, sex, co-morbidities, stone size, and renal anomaly type as co-variates. Multivariate logistic regression of factors (mode of treatment [PCNL or RIRS], comorbidities, stone size) and their effects on outcomes of stone-free rate (SFR), need to abandon surgery due to intraoperative difficulty, postoperative hematuria and sepsis and were analyzed when applicable.
Results: After PSM, there were a total of 127 pairs in each group. Overall, PCNL conferred a higher SFR compared to RIRS (OR=3.69, 95%-CI=1.91-7.46, p<0.001), particularly in HSK (OR=3.33, 95%-CI=1.22-9.99, p=0.023), and ectopic kidneys (OR=18.10, 95%-CI=3.62-147.63, p=0.002), with no significant difference in malrotated kidneys. There was no significant difference in post-operative sepsis observed. Surgery was abandoned more often in RIRS than PCNL (6.3% vs 0%, p=0.014). Although PSM provides a robust analysis due to baseline differences in the unmatched cohorts, this study was limited by an inevitable degree of selection bias.
Conclusions: While both modalities are safe and efficacious, PCNL yields better SFR than RIRS in patients with anomalous kidneys, with no difference in post-operative sepsis rates. Patients may benefit from personalised management best carried out in high volume endourology centers.
Source of Funding: NA
We aim to compare the safety, outcomes and complications of retrograde intrarenal surgery (RIRS) versus percutaneous nephrolithotomy (PCNL) in patients with urolithiasis in anomalous kidneys.
Methods: A propensity score-matched pair analysis (PSM) was performed on pooled patient data from 20 centers. 569 patients with anomalous kidneys (Horseshoe kidney(HSK), ectopic kidney, malrotated kidney) and urolithiasis who received either PCNL or RIRS as the primary modality of intervention from 2010 to 2020 were analyzed. Patients were matched based on calculated propensity scores by a regression model using age, sex, co-morbidities, stone size, and renal anomaly type as co-variates. Multivariate logistic regression of factors (mode of treatment [PCNL or RIRS], comorbidities, stone size) and their effects on outcomes of stone-free rate (SFR), need to abandon surgery due to intraoperative difficulty, postoperative hematuria and sepsis and were analyzed when applicable.
Results: After PSM, there were a total of 127 pairs in each group. Overall, PCNL conferred a higher SFR compared to RIRS (OR=3.69, 95%-CI=1.91-7.46, p<0.001), particularly in HSK (OR=3.33, 95%-CI=1.22-9.99, p=0.023), and ectopic kidneys (OR=18.10, 95%-CI=3.62-147.63, p=0.002), with no significant difference in malrotated kidneys. There was no significant difference in post-operative sepsis observed. Surgery was abandoned more often in RIRS than PCNL (6.3% vs 0%, p=0.014). Although PSM provides a robust analysis due to baseline differences in the unmatched cohorts, this study was limited by an inevitable degree of selection bias.
Conclusions: While both modalities are safe and efficacious, PCNL yields better SFR than RIRS in patients with anomalous kidneys, with no difference in post-operative sepsis rates. Patients may benefit from personalised management best carried out in high volume endourology centers.
Source of Funding: NA

.jpg)
.jpg)