Back
Poster, Podium & Video Sessions
Moderated Poster
MP16: Health Services Research: Quality Improvement & Patient Safety I
MP16-11: Validation of a Single Item Screening Measure of Urologic Patient Financial Distress
Friday, May 13, 2022
4:30 PM – 5:45 PM
Location: Room 228
Daniel Au*, Jared Starkey, Jessica Hamilton, Jeffery Thompson, William Parker, Kansas City, KS

Daniel M. Au, MD
The University of Kansas Medical Center
Poster Presenter(s)
Introduction: Financial toxicity is an area of increasing focus in healthcare generally and within urologic practice. Patients with financial toxicity are more likely to forgo or delay care with negative clinical consequences. There is little guidance on how to identify patients with financial distress. The COmprehensive Score for financial Toxicity (COST) is a previously validated 12 item measure of healthcare associated financial toxicity. COST is scored from 0 to 44 with lower scores equaling worse financial toxicity. Given questionnaire burden and visit time limitations, multi-item surveys are difficult to utilize. This study aimed to validate a single item screening measure of financial toxicity among a cross section of urology patients.
Methods: All patients completing robotic assisted prostatectomy, transurethral resection of bladder tumor, radical cystectomy, holmium laser enucleation of prostate, intravesical chemodenervation, ureteroscopy laser lithotripsy, and ureteral stent exchange at a single academic medical center during study period were offered enrollment. 182 patients enrolled, peri-op COST surveys were obtained with the following single item measure: “Please indicate the number that best describes how much financial stress you have been experiencing in the past week, including today, on a scale from 0 (no financial distress) to 10 (extreme financial distress).” Pearson’s correlation coefficient compared single item performance to COST.
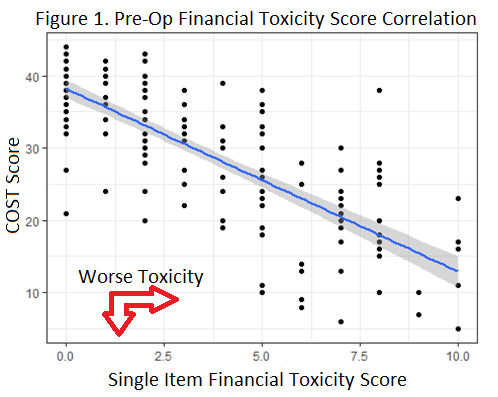
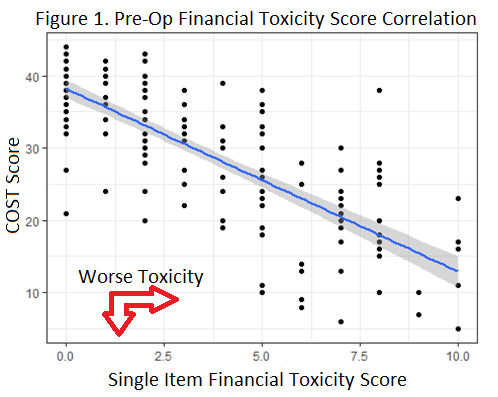
Results: Pre-operatively 69.2% (126), 23.6% (43), and 7.1% (13) of patients had COST scores indicating no/mild, moderate (COST 14-25), and severe (COST =13) financial toxicity respectively. Post-operatively 72.5% (132), 22.5% (41), and 5.9% (9) of patients had COST scores of no/mild, moderate, and severe financial toxicity respectively. Single item measure strongly correlated with COST (r=-0.80, 95% CI -0.73,-0.84) pre-op (Figure 1) and post-op (r=-0.75, 95% CI -0.68,-0.81). A cut point of single item score =5 had a 77% sensitivity and 85% specificity for moderate to severe financial toxicity.
Conclusions: There are inadequate clinical support tools to assess patients for financial toxicity. Presence and degree of financial toxicity is a clinically relevant metric. This single item measure is a sensitive and practical screening tool for urologic clinical practice.
Source of Funding: None
Methods: All patients completing robotic assisted prostatectomy, transurethral resection of bladder tumor, radical cystectomy, holmium laser enucleation of prostate, intravesical chemodenervation, ureteroscopy laser lithotripsy, and ureteral stent exchange at a single academic medical center during study period were offered enrollment. 182 patients enrolled, peri-op COST surveys were obtained with the following single item measure: “Please indicate the number that best describes how much financial stress you have been experiencing in the past week, including today, on a scale from 0 (no financial distress) to 10 (extreme financial distress).” Pearson’s correlation coefficient compared single item performance to COST.
Results: Pre-operatively 69.2% (126), 23.6% (43), and 7.1% (13) of patients had COST scores indicating no/mild, moderate (COST 14-25), and severe (COST =13) financial toxicity respectively. Post-operatively 72.5% (132), 22.5% (41), and 5.9% (9) of patients had COST scores of no/mild, moderate, and severe financial toxicity respectively. Single item measure strongly correlated with COST (r=-0.80, 95% CI -0.73,-0.84) pre-op (Figure 1) and post-op (r=-0.75, 95% CI -0.68,-0.81). A cut point of single item score =5 had a 77% sensitivity and 85% specificity for moderate to severe financial toxicity.
Conclusions: There are inadequate clinical support tools to assess patients for financial toxicity. Presence and degree of financial toxicity is a clinically relevant metric. This single item measure is a sensitive and practical screening tool for urologic clinical practice.
Source of Funding: None

.jpg)
.jpg)