Back
Poster, Podium & Video Sessions
Moderated Poster
MP17: Pediatric Urology: Upper & Lower Urinary Tract
MP17-13: Evaluation of Renal Function in Pediatric Patients Undergoing Urologic Surgery Using NSQIP-P Data
Friday, May 13, 2022
4:30 PM – 5:45 PM
Location: Room 225
Victor Chalfant*, Carlos Riveros, Andrew Stec, Jacksonville, FL
- VC
Poster Presenter(s)
Introduction: Renal protection is a frequent indication for major pediatric urologic surgery; however, its preoperative assessment is not routinely performed in many cases. Using the NSQIP-Pediatric data, this manuscript explores the incidence of preoperative renal function testing and stratifies outcomes for major pediatric urologic surgeries.
Methods: Cases with complete data were identified in the 2012-2019 NSQIP-P database using CPT codes for ureteroneocystostomy, nephrectomy, complicated pyeloplasty, cutaneous appendico-vesicostomy, ureteroureterostomy and bladder exstrophy closure. For simplicity, GFR was calculated using the Bedside Schwartz Equation (=2 years of age): eGFR=0.413x(height/Cr). Abnormal renal function was defined as Cr =0.5mg/dL ( <2 years) and a GFR <90mL/min (=2 years of age).
NSQIP complications were assessed using Fisher's exact test and analysis was conducted using SPSS with p-values of <0.05 significant.
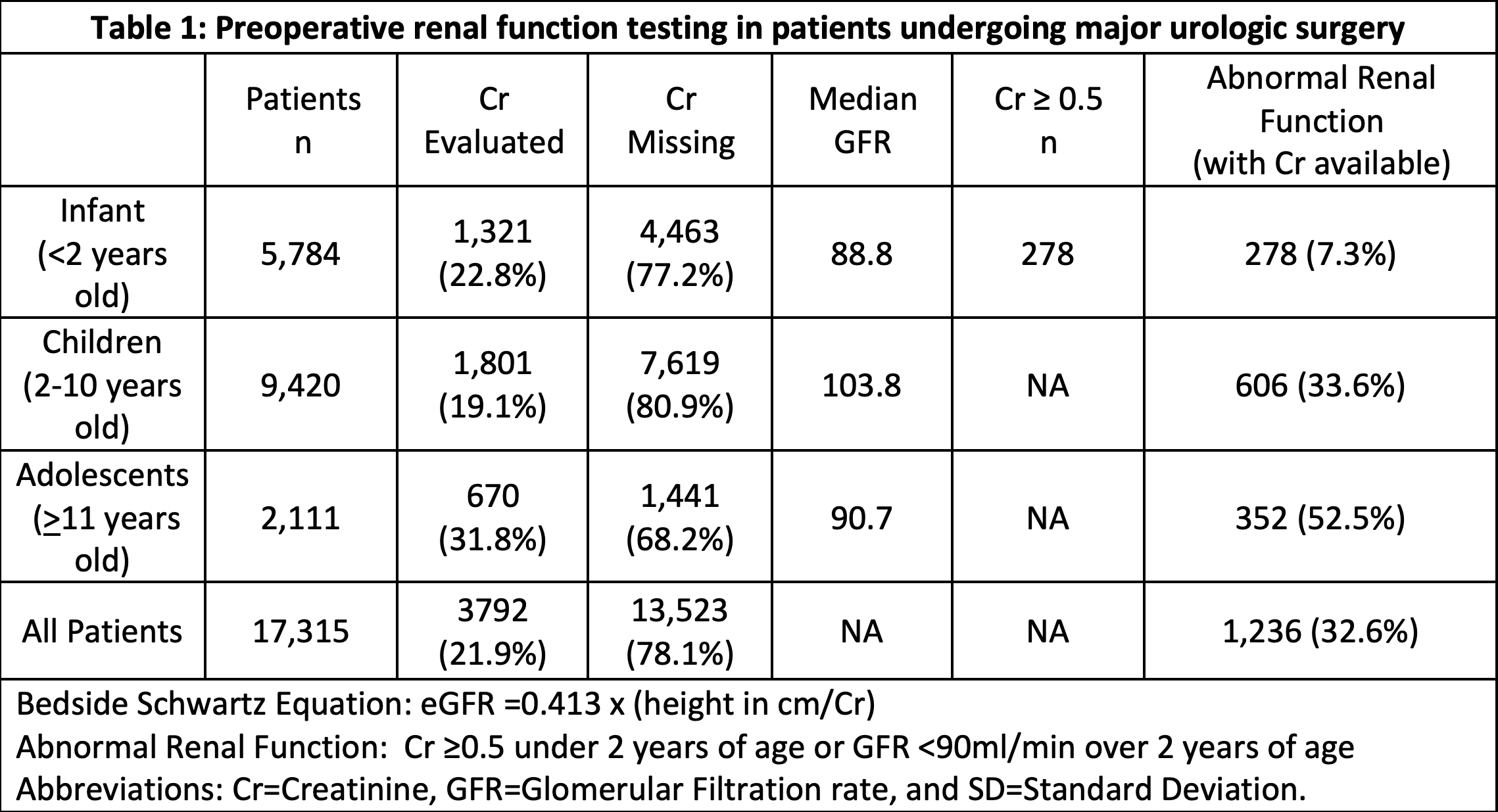
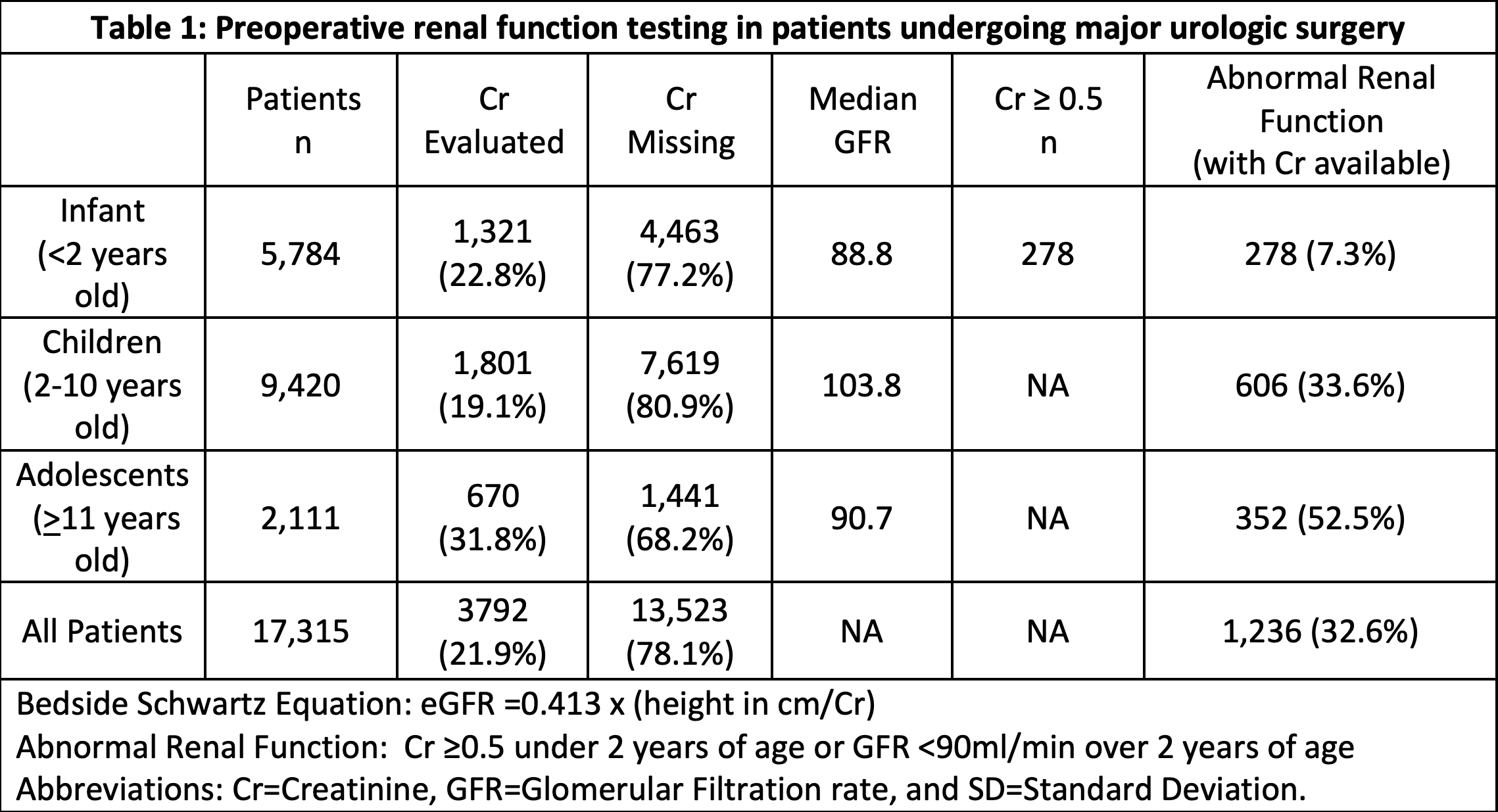
Results: 17,315 patients were included; and only 3,792 (21.9%) had Cr values within 30-days prior to surgery (Table 1). Abnormal renal function was demonstrated in 7.3% of infants, 33.6% of children, and 52.5% of adolescents based on the defined criteria. Statistical analysis demonstrated that patients with preoperative creatinine values were significantly ( < 0.001) more likely to experience readmission (10.2% vs 5.8%), reoperation (3.7% vs 1.6%), organ/space surgical site infection (0.9% vs 0.4%), transfusion (4.0% vs 0.5%), renal insufficiency (0.8% vs 0.1%), systemic sepsis (1.5% vs 0.6%), and urinary tract infection (5.1% vs 3.6%).
Conclusions: In this NSQIP-P population only 21.9% of patients had Cr values assessed prior to major urologic surgery with 1 in 3 patients checked having evidence of decreased renal function. These numbers suggest undertesting and underreporting of issues with renal function in a cohort at high risk for renal issues. There was also a significant likelihood that patients with renal function testing were higher risk and experienced complications at a higher rate. Pathways and guidelines for major pediatric urologic cases have room for improvement, starting with more widespread adoption of preoperative renal function testing and heightened surveillance in those with abnormal renal function in the post-procedure timeframe.
Source of Funding: N/A
Methods: Cases with complete data were identified in the 2012-2019 NSQIP-P database using CPT codes for ureteroneocystostomy, nephrectomy, complicated pyeloplasty, cutaneous appendico-vesicostomy, ureteroureterostomy and bladder exstrophy closure. For simplicity, GFR was calculated using the Bedside Schwartz Equation (=2 years of age): eGFR=0.413x(height/Cr). Abnormal renal function was defined as Cr =0.5mg/dL ( <2 years) and a GFR <90mL/min (=2 years of age).
NSQIP complications were assessed using Fisher's exact test and analysis was conducted using SPSS with p-values of <0.05 significant.
Results: 17,315 patients were included; and only 3,792 (21.9%) had Cr values within 30-days prior to surgery (Table 1). Abnormal renal function was demonstrated in 7.3% of infants, 33.6% of children, and 52.5% of adolescents based on the defined criteria. Statistical analysis demonstrated that patients with preoperative creatinine values were significantly ( < 0.001) more likely to experience readmission (10.2% vs 5.8%), reoperation (3.7% vs 1.6%), organ/space surgical site infection (0.9% vs 0.4%), transfusion (4.0% vs 0.5%), renal insufficiency (0.8% vs 0.1%), systemic sepsis (1.5% vs 0.6%), and urinary tract infection (5.1% vs 3.6%).
Conclusions: In this NSQIP-P population only 21.9% of patients had Cr values assessed prior to major urologic surgery with 1 in 3 patients checked having evidence of decreased renal function. These numbers suggest undertesting and underreporting of issues with renal function in a cohort at high risk for renal issues. There was also a significant likelihood that patients with renal function testing were higher risk and experienced complications at a higher rate. Pathways and guidelines for major pediatric urologic cases have room for improvement, starting with more widespread adoption of preoperative renal function testing and heightened surveillance in those with abnormal renal function in the post-procedure timeframe.
Source of Funding: N/A

.jpg)
.jpg)