Back
Poster, Podium & Video Sessions
Best Poster Award
MP17: Pediatric Urology: Upper & Lower Urinary Tract
MP17-14: Is Excretory Phase Computerized Tomography Important for Evaluation of High Grade Renal Trauma?: Results from the Traumatic Renal Injury Collaboration for Kids (TRICK)
Friday, May 13, 2022
4:30 PM – 5:45 PM
Location: Room 225
Ching Man Carmen Tong*, Birmingham, AL, Jacob Lucas, Philadelphia, PA, Albert Lee, Washington D.C., DC, Vinaya Bhatia, Houston, TX, Benjamin Abelson, Nashville, TN, Christopher Long, Dana Weiss, Philadelphia, PA, Christina Ho, Washington D.C., DC, Jeffrey Ellis, Philadelphia, PA, Harold Lovvorn, Nashville, TN, Teressa Duong, Birmingham, AL, Jonathan Gerber, Houston, TX, Gabriella Crane, Nashville, TN, Xiaoyi Zhuo, Houston, TX, Robert Russell, Birmingham, AL, Soo Kim, Ming-Hsien Wang, Houston, TX, Douglass Clayton, Nashville, TN, David Kitchens, Birmingham, AL
Ching Man Carmen Tong, DO
pediatric urologist
University of Alabama at Birmingham
Poster Presenter(s)
Introduction: Currently no standardized imaging guidelines exist for pediatric kidney trauma. While excretory phase computerized tomography (EPCT) scans are recommended in adults, the necessity of EPCT remains undefined in children. TRICK is a multi-institutional consortium to investigate pediatric renal trauma in the U.S. In this report, we hypothesized that outcomes and recovery of traumatic renal injury at TRICK centers are independent of EPCT use.
Methods: We reviewed retrospective data from 5 pediatric trauma centers from 2007-2020. Patients <18 years old with high grade renal trauma, defined as American Association for the Surgery of Trauma (AAST) grade III or higher, were included. We collected data on imaging modalities and clinical course. Primary outcome of the study was rate of delayed surgical (endoscopic stent placement or nephrectomy) or radiologic intervention such as percutaneous drains or angiographic embolization.
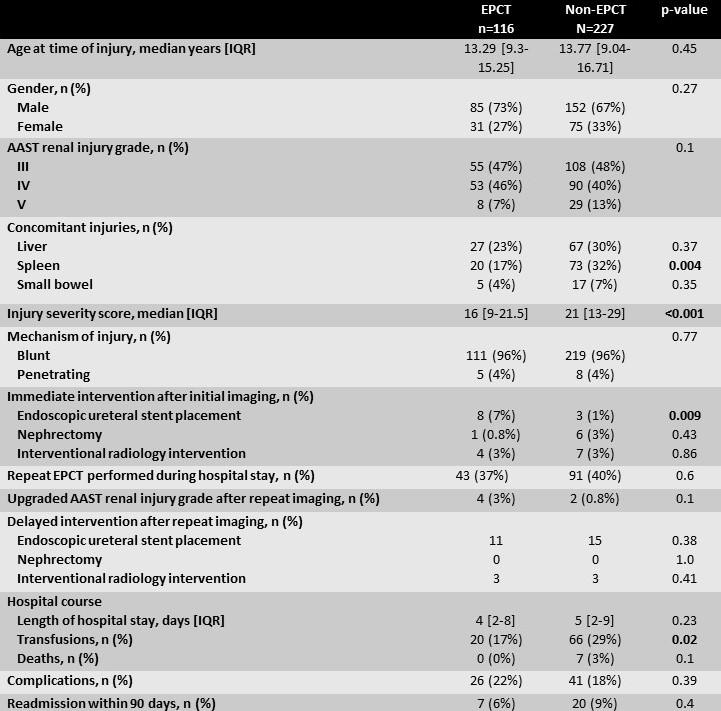
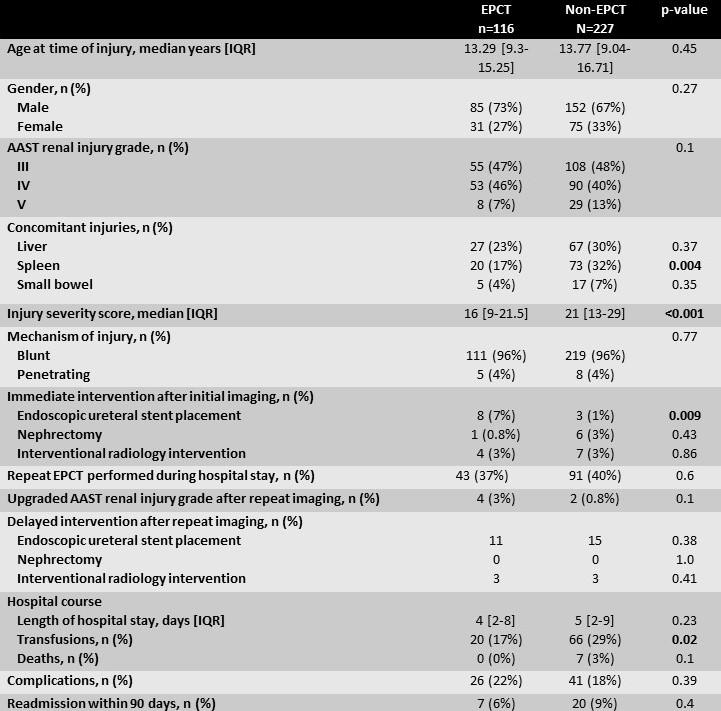
Results: 343 children sustained high-grade renal trauma. Comparison between children with EPCT during initial evaluation (n=116, 34%) and those who received a contrasted CT without excretory phase (n=227, 66%) showed no difference in patient demographics, mechanism or grades of injury. Children in the non-EPCT had higher median injury severity score (p < 0.001) and splenic injuries (p=0.004). After initial evaluation with EPCT, more children underwent endoscopic ureteral stent placement (7%) compared to those with non-EPCT (1%, p=0.009). Length of hospital and discharge status were not statistically different although more children with non-EPCT imaging received transfusions (p=0.02). Finally, compared to those with initial EPCT, patients with initial non-EPCT did not undergo more delayed imaging or experience higher rates of delayed surgical or radiologic intervention. Complications or readmission rates within 90 days were not statistically different.
Conclusions: TRICK demonstrates that high grade renal trauma can be initially evaluated with non-EPCT with no difference in surgical outcomes or readmission rates. This study will help drive future prospective protocols to select patients who may benefit from multi-phase CT while minimizing radiation risk to those with self-resolving injuries.
Source of Funding: None
Methods: We reviewed retrospective data from 5 pediatric trauma centers from 2007-2020. Patients <18 years old with high grade renal trauma, defined as American Association for the Surgery of Trauma (AAST) grade III or higher, were included. We collected data on imaging modalities and clinical course. Primary outcome of the study was rate of delayed surgical (endoscopic stent placement or nephrectomy) or radiologic intervention such as percutaneous drains or angiographic embolization.
Results: 343 children sustained high-grade renal trauma. Comparison between children with EPCT during initial evaluation (n=116, 34%) and those who received a contrasted CT without excretory phase (n=227, 66%) showed no difference in patient demographics, mechanism or grades of injury. Children in the non-EPCT had higher median injury severity score (p < 0.001) and splenic injuries (p=0.004). After initial evaluation with EPCT, more children underwent endoscopic ureteral stent placement (7%) compared to those with non-EPCT (1%, p=0.009). Length of hospital and discharge status were not statistically different although more children with non-EPCT imaging received transfusions (p=0.02). Finally, compared to those with initial EPCT, patients with initial non-EPCT did not undergo more delayed imaging or experience higher rates of delayed surgical or radiologic intervention. Complications or readmission rates within 90 days were not statistically different.
Conclusions: TRICK demonstrates that high grade renal trauma can be initially evaluated with non-EPCT with no difference in surgical outcomes or readmission rates. This study will help drive future prospective protocols to select patients who may benefit from multi-phase CT while minimizing radiation risk to those with self-resolving injuries.
Source of Funding: None

.jpg)
.jpg)