Back
Poster, Podium & Video Sessions
Moderated Poster
MP17: Pediatric Urology: Upper & Lower Urinary Tract
MP17-15: Pediatric Inguinal Hernia Management Between Pediatric Surgeons and Pediatric Urologists
Friday, May 13, 2022
4:30 PM – 5:45 PM
Location: Room 225
Teressa Duong*, Vincent Mortellaro, David Kitchens, David Joseph, Ching Man Carmen Tong, Birmingham, AL
Poster Presenter(s)
Introduction:
Introduction: Pediatric inguinal hernias are managed by both pediatric surgeons and urologists. While the training process for the subspecialties is different, there is little data that examine differences in patient demographics, operative details, and patient outcomes. In this study, we aim to investigate variations of these factors for open pediatric inguinal hernia repairs (IHR) between pediatric surgeons and pediatric urologists.
Objective: To investigate differences between patient demographics, operative details, and patient outcomes for open pediatric inguinal hernia repairs between pediatric surgeons and pediatric urologists.
Methods: We received IRB approval from our institution and performed a retrospective chart review on patients between 0-18 years old who received an initial open IHR between [2015-2020]. Exclusion criteria includes laparoscopic repairs and recurrent IHR. We collected data on demographics, operative details, and clinical outcomes including complications and recurrences. Statistical analysis was performed using SPSSv.27.
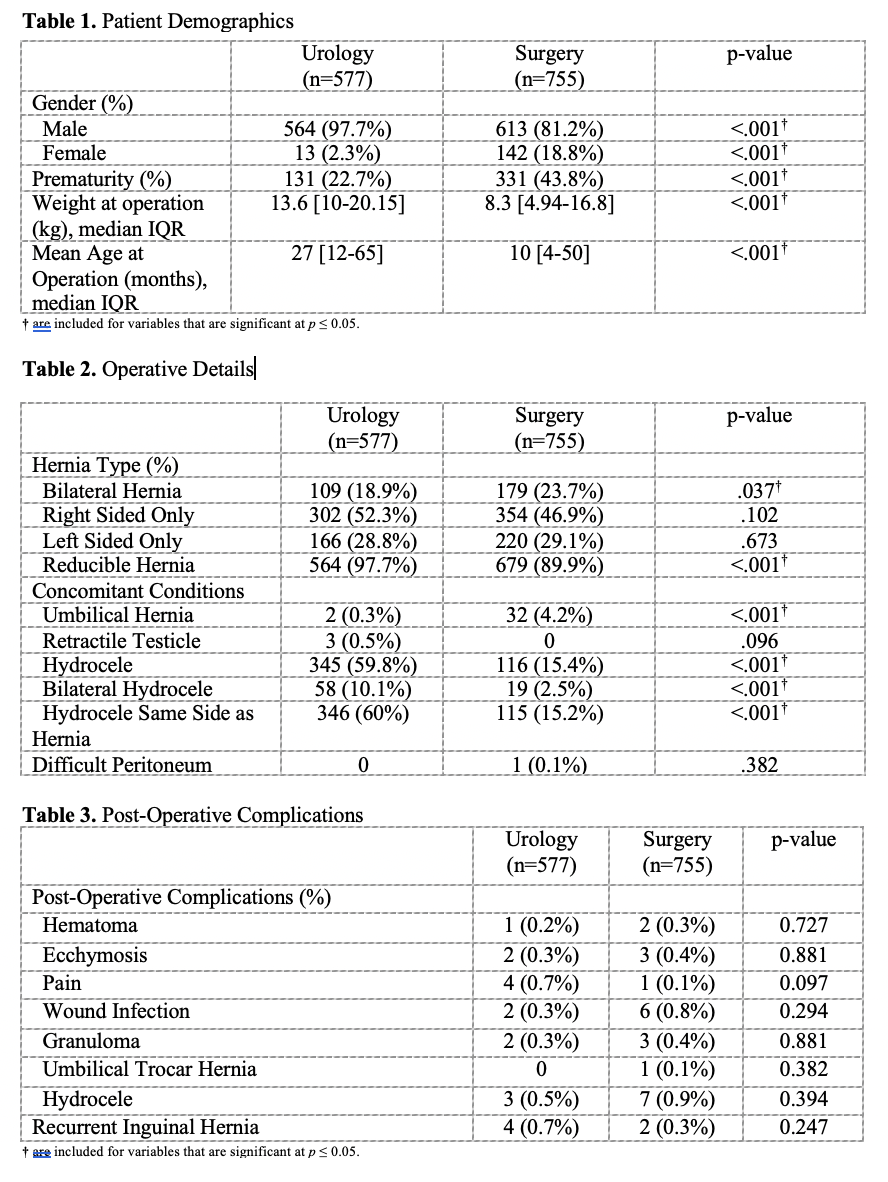
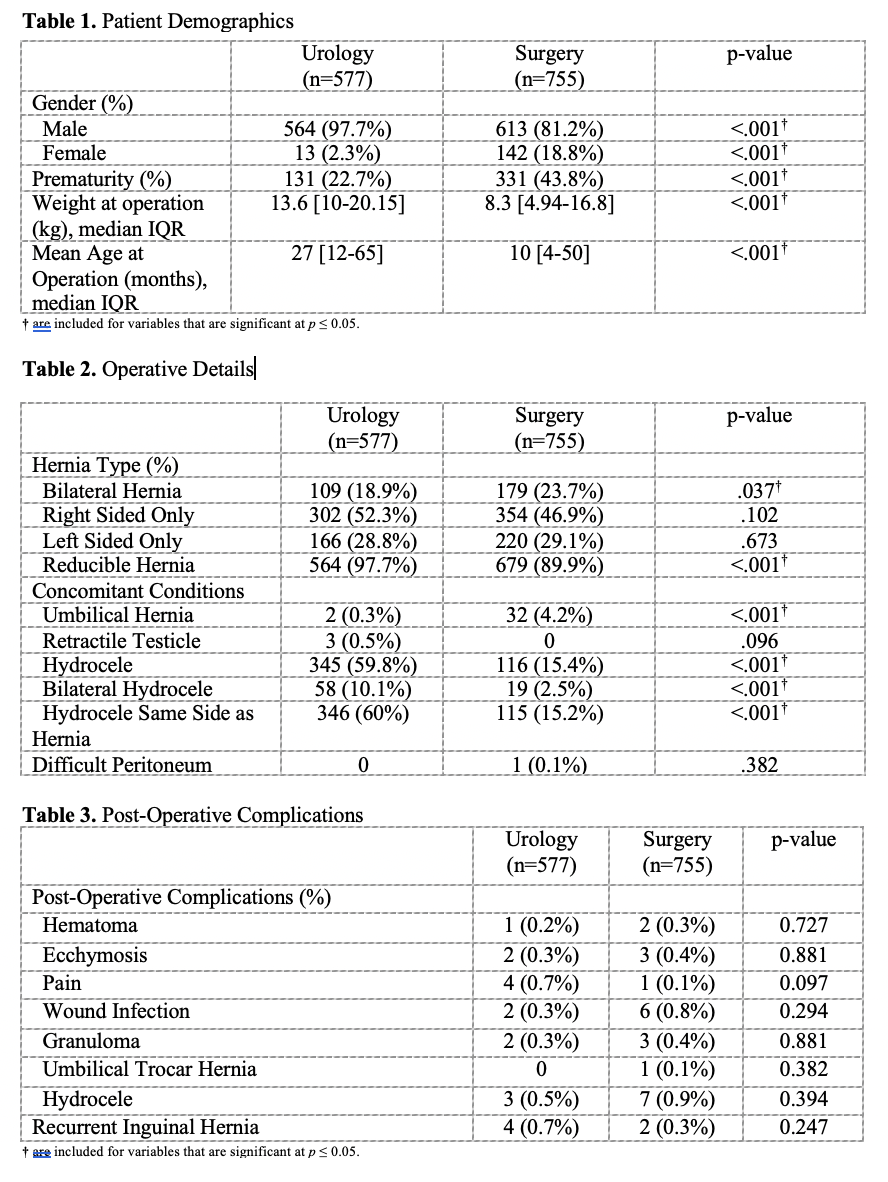
Results: A total of 1332 patients during the study period were included, with 755 performed by 6 pediatric surgeons and 577 by 3 pediatric urologists. Pediatric surgeons repaired more inguinal hernias in females and patients with a history of prematurity (p < .001). Median age at time of operation for surgeons and urologist were 10 and 27 months old, respectively (p < .001). Urology repaired significantly less bilateral hernias and incarcerated hernias than surgery (p = .037). Urology repairs had significantly more concomitant hydroceles than surgery (p < 0.001). There were no significant differences in patient outcomes including recurrent hernias, infections, and granulomas.
Conclusions: : Our study demonstrates that IHR performed by pediatric surgery and pediatric urology were equally successful. Patient demographics, hernia characteristics, and concomitant conditions differ significantly between pediatric urologists and pediatric surgeons, although this is likely due to differences in referral patterns in our community. Overall, there were no significant differences in patient outcomes between the two specialties.
Source of Funding: None
Introduction: Pediatric inguinal hernias are managed by both pediatric surgeons and urologists. While the training process for the subspecialties is different, there is little data that examine differences in patient demographics, operative details, and patient outcomes. In this study, we aim to investigate variations of these factors for open pediatric inguinal hernia repairs (IHR) between pediatric surgeons and pediatric urologists.
Objective: To investigate differences between patient demographics, operative details, and patient outcomes for open pediatric inguinal hernia repairs between pediatric surgeons and pediatric urologists.
Methods: We received IRB approval from our institution and performed a retrospective chart review on patients between 0-18 years old who received an initial open IHR between [2015-2020]. Exclusion criteria includes laparoscopic repairs and recurrent IHR. We collected data on demographics, operative details, and clinical outcomes including complications and recurrences. Statistical analysis was performed using SPSSv.27.
Results: A total of 1332 patients during the study period were included, with 755 performed by 6 pediatric surgeons and 577 by 3 pediatric urologists. Pediatric surgeons repaired more inguinal hernias in females and patients with a history of prematurity (p < .001). Median age at time of operation for surgeons and urologist were 10 and 27 months old, respectively (p < .001). Urology repaired significantly less bilateral hernias and incarcerated hernias than surgery (p = .037). Urology repairs had significantly more concomitant hydroceles than surgery (p < 0.001). There were no significant differences in patient outcomes including recurrent hernias, infections, and granulomas.
Conclusions: : Our study demonstrates that IHR performed by pediatric surgery and pediatric urology were equally successful. Patient demographics, hernia characteristics, and concomitant conditions differ significantly between pediatric urologists and pediatric surgeons, although this is likely due to differences in referral patterns in our community. Overall, there were no significant differences in patient outcomes between the two specialties.
Source of Funding: None

.jpg)
.jpg)
