Back
Poster, Podium & Video Sessions
Moderated Poster
MP17: Pediatric Urology: Upper & Lower Urinary Tract
MP17-17: Prediction of Wilms' tumor relapse risk using genetic and metabolomic markers
Friday, May 13, 2022
4:30 PM – 5:45 PM
Location: Room 225
Ahmed Abdelhalim*, Mariam AbdelMonem, Asmaa Ahmed, Amira Awadalla, Mohamed Abdelhameed, Mansoura, Egypt, Ranim Mahmoud, Masnoura, Egypt, Om Ali El-khawaga, Ashraf Hafez, Mansoura, Egypt
- AA
Ahmed Abdelhalim, MD
Mansoura University Urology and Nephrology Center
Poster Presenter(s)
Introduction: Although the survival of children with Wilms' tumor (WT) has substantially improved thanks to multimodal management and risk-stratification, disease relapse still carries a dismal prognosis. We aim to investigate the prognostic value of several genetic and metabolomic markers and test their association with the risk of WT relapse.
Methods: The study included 51 children treated for WT at a tertiary center between 2001 and 2019. Of those, 23 patients had disease relapse and 28 remained free of relapse at last follow-up. Patients were treated according to the Children’s Oncology Group protocols. Patients with syndromic WT, anaplastic histology and those with less than 2 years of follow-up were excluded. Autologous normal renal tissue from 20 patients served as control. Total RNA was isolated from formalin-fixed paraffin embedded blocks from tumors and normal renal tissue. The expression of the following genes was assessed using quantitative real-time PCR (qRT-PCR): WT1, HOXA5, SLC22A18, MYC, HIF1a and b-FGF genes. The expression of the target genes was normalized to Glyceraldehyde 3-phosphate dehydrogenase (GAPDH) as an endogenous control. The level of expression of tested genes was compared between patients who experienced disease relapse, patients who remained free of relapse and healthy control.
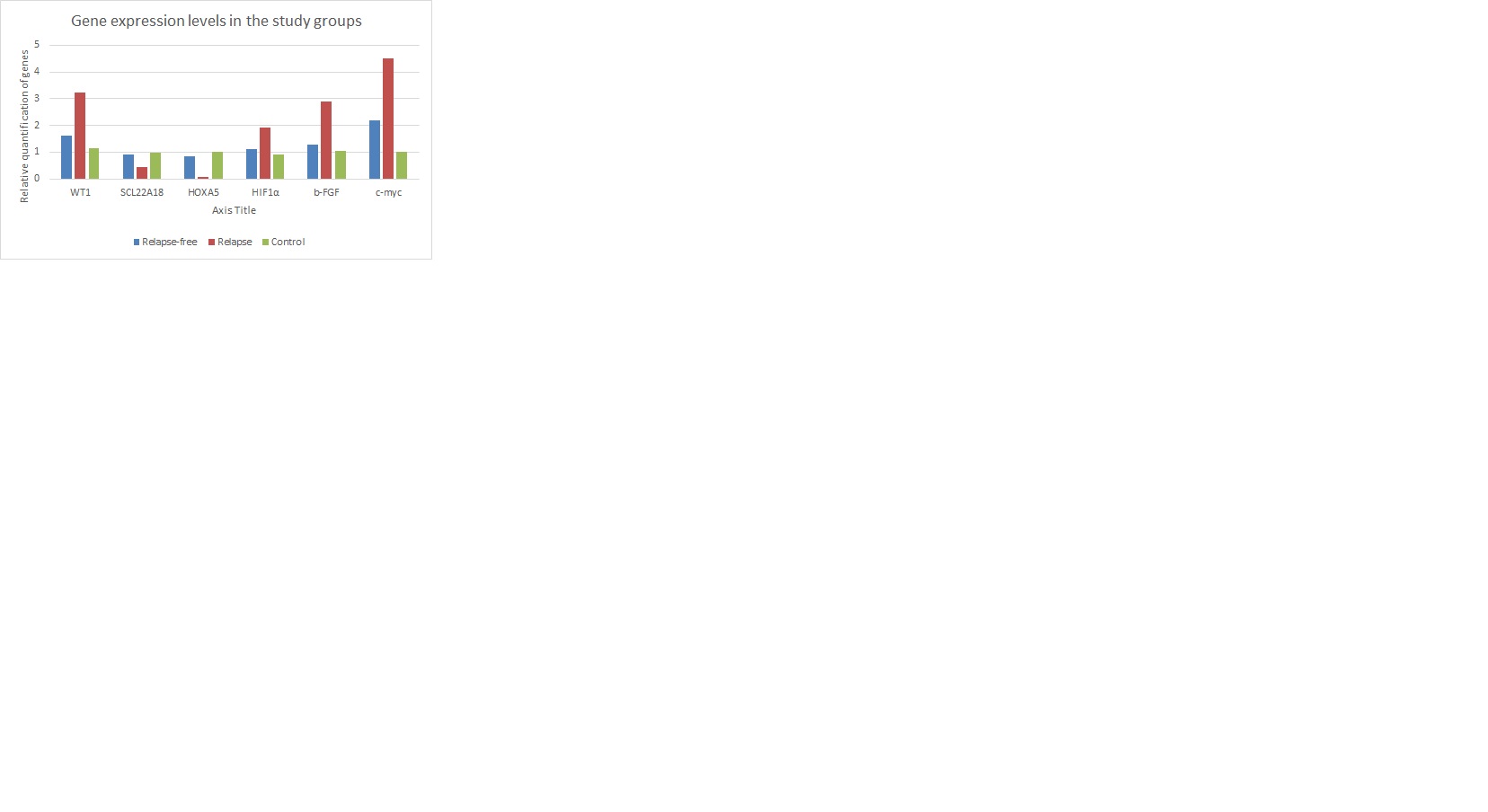
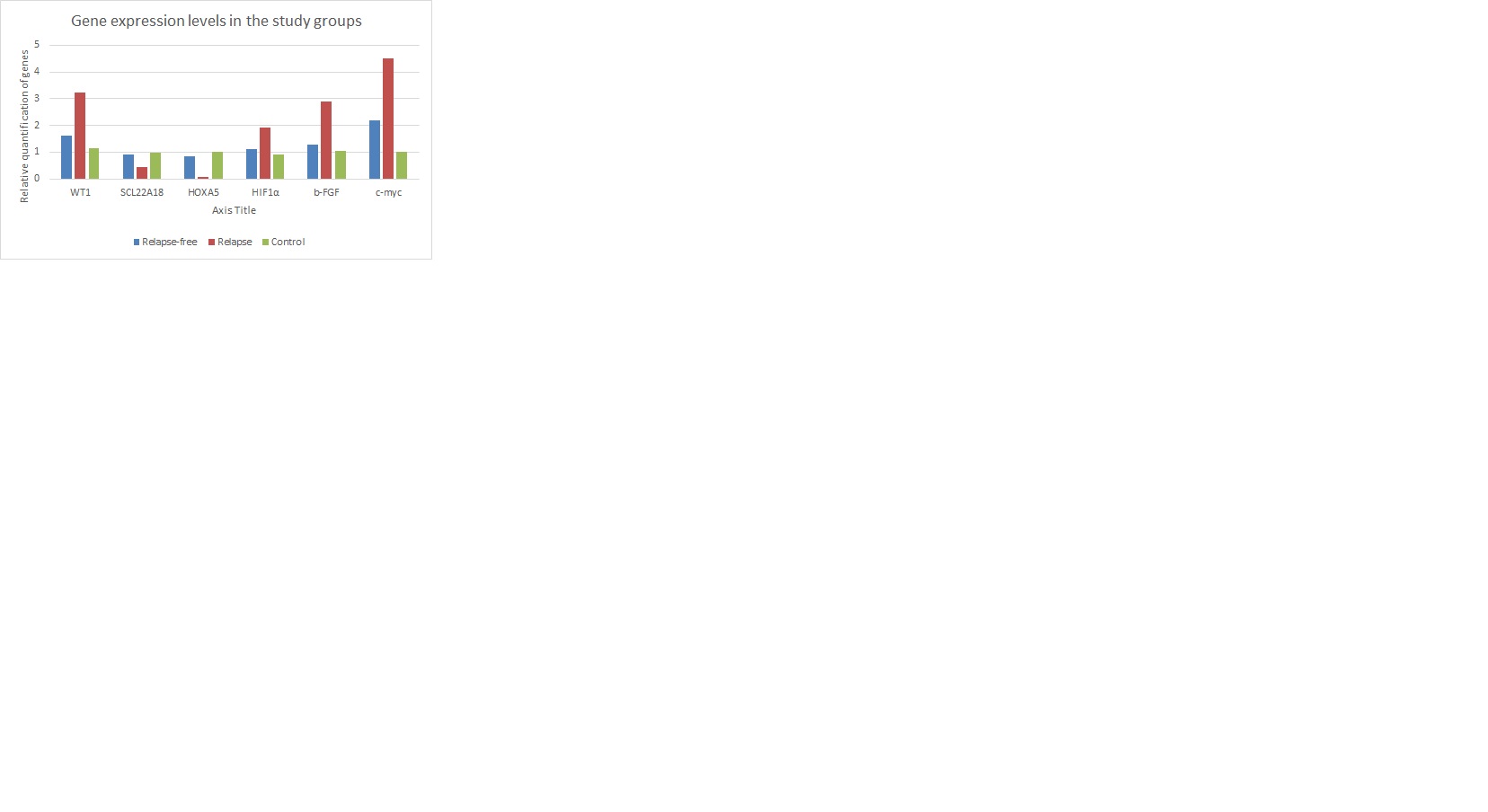
Results: Mean patient age at presentation was 3.9 ± 3.2 years and 27 (52.9%) were males. The majority of patients (76.5%) had stage I disease. Age at presentation, gender and tumor stage were not significantly different between the relapse and relapse-free groups (p=0.131, 0.22 and 0.146; respectively). Tumors that relapsed expressed significantly higher levels of WT1, HIF1a, b-FGF and c-myc (p < 0.001 for all). In contrast, gene expression levels of SLC22A18 and HOXA5 (p < 0.001 for both) were significantly lower in patients who suffered disease relapse (figure).
Conclusions: Wilms’ tumors with higher expression levels of WT1, HIF1 a, b-FGF and c-myc and lower expression levels of SLC22A18 and HOXA5 are at increased risk of disease relapse. These genetic and metabolomic markers can serve as future prognostic predictors and help stratify patients for treatment and follow-up regimens.
Source of Funding: The study received funding from the Science, Technology & Innovation Funding Authority (STIFA) project number 43363.
Methods: The study included 51 children treated for WT at a tertiary center between 2001 and 2019. Of those, 23 patients had disease relapse and 28 remained free of relapse at last follow-up. Patients were treated according to the Children’s Oncology Group protocols. Patients with syndromic WT, anaplastic histology and those with less than 2 years of follow-up were excluded. Autologous normal renal tissue from 20 patients served as control. Total RNA was isolated from formalin-fixed paraffin embedded blocks from tumors and normal renal tissue. The expression of the following genes was assessed using quantitative real-time PCR (qRT-PCR): WT1, HOXA5, SLC22A18, MYC, HIF1a and b-FGF genes. The expression of the target genes was normalized to Glyceraldehyde 3-phosphate dehydrogenase (GAPDH) as an endogenous control. The level of expression of tested genes was compared between patients who experienced disease relapse, patients who remained free of relapse and healthy control.
Results: Mean patient age at presentation was 3.9 ± 3.2 years and 27 (52.9%) were males. The majority of patients (76.5%) had stage I disease. Age at presentation, gender and tumor stage were not significantly different between the relapse and relapse-free groups (p=0.131, 0.22 and 0.146; respectively). Tumors that relapsed expressed significantly higher levels of WT1, HIF1a, b-FGF and c-myc (p < 0.001 for all). In contrast, gene expression levels of SLC22A18 and HOXA5 (p < 0.001 for both) were significantly lower in patients who suffered disease relapse (figure).
Conclusions: Wilms’ tumors with higher expression levels of WT1, HIF1 a, b-FGF and c-myc and lower expression levels of SLC22A18 and HOXA5 are at increased risk of disease relapse. These genetic and metabolomic markers can serve as future prognostic predictors and help stratify patients for treatment and follow-up regimens.
Source of Funding: The study received funding from the Science, Technology & Innovation Funding Authority (STIFA) project number 43363.

.jpg)
.jpg)