Back
Poster, Podium & Video Sessions
Moderated Poster
MP18: Urodynamics/Lower Urinary Tract Dysfunction/Female Pelvic Medicine: Non-neurogenic Voiding Dysfunction I
MP18-13: The Sensation Meter: A Novel Non-Invasive Approach to Understanding Bladder Sensation Events
Friday, May 13, 2022
4:30 PM – 5:45 PM
Location: Room 222
Elizabeth Rourke*, New Orleans, LA, W. Stuart Reynolds, Nashville, TN
- ER
Elizabeth Ann Rourke, DO, MPH
Assistant Professor of Clinical Urology
Louisiana State University Medical Center
Poster Presenter(s)
Introduction: Overactive bladder (OAB) is a defined as a symptom syndrome (urinary urgency, frequency and/or nocturia and urinary incontinence) that presents in varying degrees in patients. The ability to define subtypes of idiopathic OAB remains unclear however, expert consensus suggests that OAB phenotypes exist that reflect different pathophysiologic characteristics. The objective of this study is to utilize a non-invasive, validated sensation-meter tool and hydration protocol in order to characterize bladder sensations in individuals with OAB.
Methods: This is prospective cohort study of adult men and women aged 18 years and older with OAB and without OAB recruited through the Vanderbilt Research Notification Distribution List. The bladder sensation meter is a touch-screen computer tablet-based application (LabView, National Instruments, Austin, TX) for self-recorded sensory data. A standardized oral hydration protocol was used, in which participants were instructed to drink two liters of Gatorade-G2® (low-sugar). The interface allows each participant to quantify his/her bladder sensation in real-time.
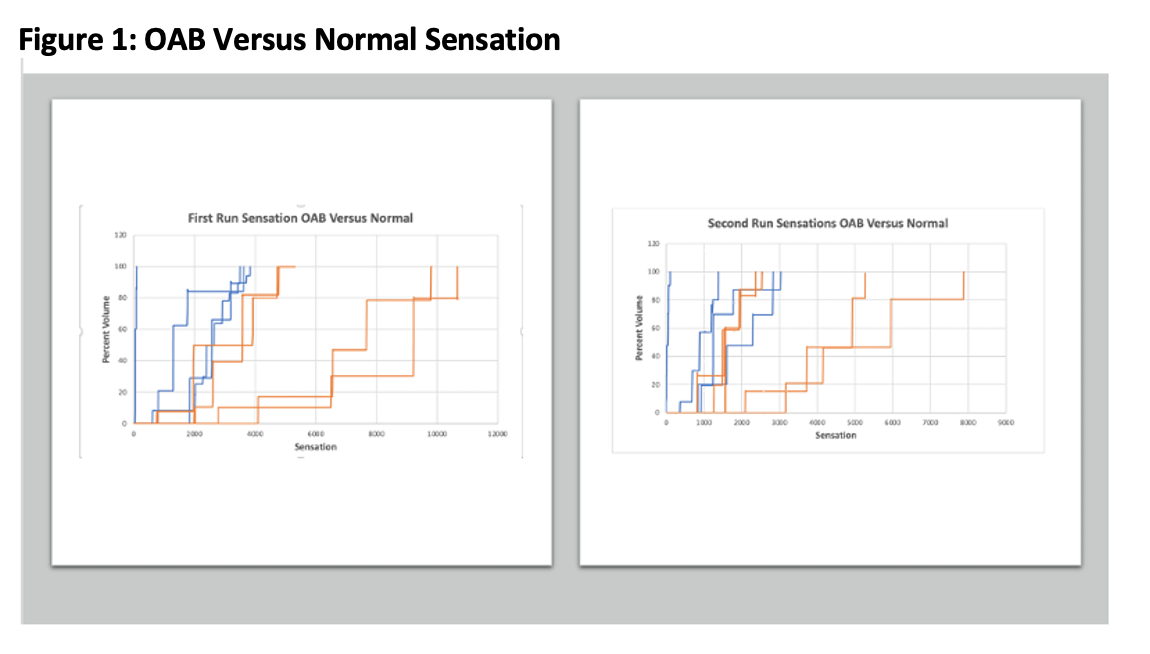
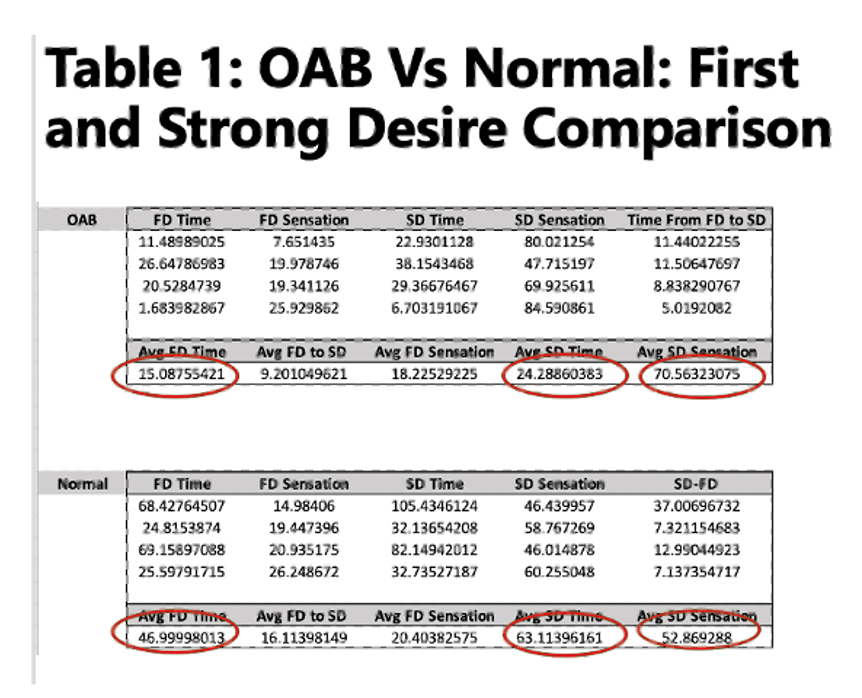
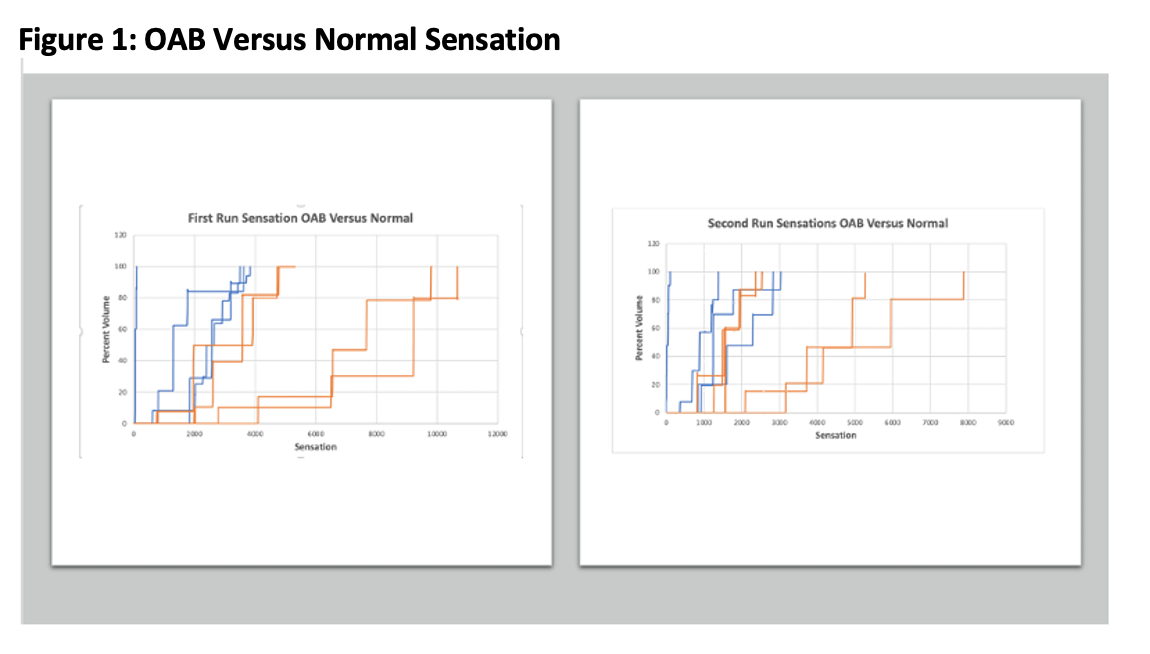
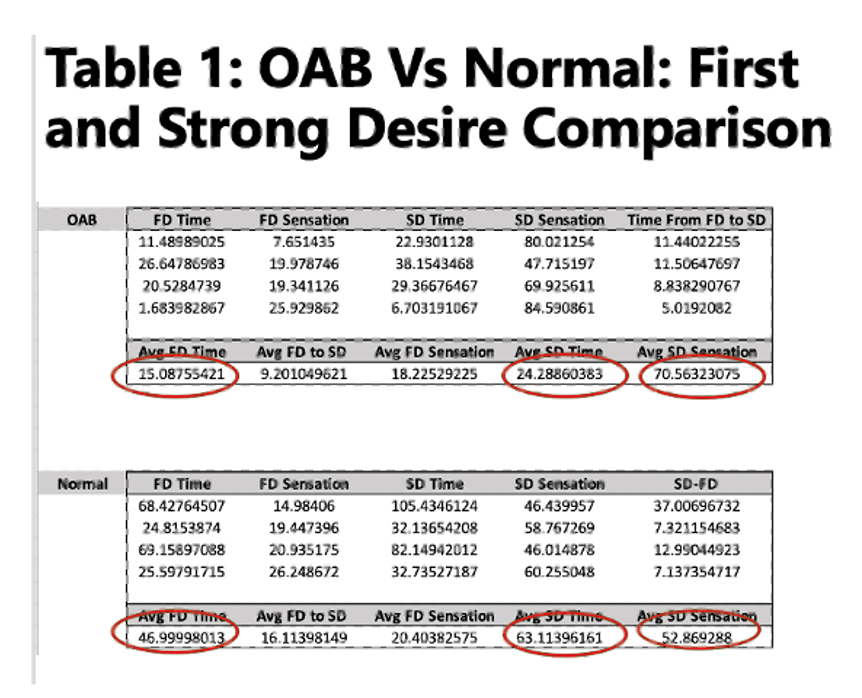
Results: Preliminary study results included 8 female subjects: 4 OAB and 4 Controls. The sensation of tingling was reported more often in OAB group compared to controls (n=7 versus n=2) and tense was reported more often in controls (n=5 versus n=0 for OAB). Only pressure and tingling were reported sensations in the OAB group. Subjects in the OAB group demonstrated shorter time intervals to first desire and strong desire as compared to controls (Table 1/Figure 1).
Conclusions: Self-recorded sensory data has demonstrated feasibility and reproducibility in healthy controls and in those with OAB and is an innovative non-invasive tool to better understand bladder sensations in subjects with OAB. This tool allows for development of sensation-capacity curves and frequency/distribution of sensation events that can be used to delineate different clinical OAB phenotypes.
Source of Funding: Vanderbilt Institute for Clinical and Translational Research Grant
Methods: This is prospective cohort study of adult men and women aged 18 years and older with OAB and without OAB recruited through the Vanderbilt Research Notification Distribution List. The bladder sensation meter is a touch-screen computer tablet-based application (LabView, National Instruments, Austin, TX) for self-recorded sensory data. A standardized oral hydration protocol was used, in which participants were instructed to drink two liters of Gatorade-G2® (low-sugar). The interface allows each participant to quantify his/her bladder sensation in real-time.
Results: Preliminary study results included 8 female subjects: 4 OAB and 4 Controls. The sensation of tingling was reported more often in OAB group compared to controls (n=7 versus n=2) and tense was reported more often in controls (n=5 versus n=0 for OAB). Only pressure and tingling were reported sensations in the OAB group. Subjects in the OAB group demonstrated shorter time intervals to first desire and strong desire as compared to controls (Table 1/Figure 1).
Conclusions: Self-recorded sensory data has demonstrated feasibility and reproducibility in healthy controls and in those with OAB and is an innovative non-invasive tool to better understand bladder sensations in subjects with OAB. This tool allows for development of sensation-capacity curves and frequency/distribution of sensation events that can be used to delineate different clinical OAB phenotypes.
Source of Funding: Vanderbilt Institute for Clinical and Translational Research Grant

.jpg)
.jpg)