Back
Poster, Podium & Video Sessions
Moderated Poster
MP18: Urodynamics/Lower Urinary Tract Dysfunction/Female Pelvic Medicine: Non-neurogenic Voiding Dysfunction I
MP18-15: Real World Male Voiding Behavior and Variability Using an Audio-Based Uroflowmetry Application
Friday, May 13, 2022
4:30 PM – 5:45 PM
Location: Room 222
Ramy Goueli*, Dallas, TX, Min Gyeong Kim, San Francisco, CA, Kenneth Goldberg, Dallas, TX, Catherine Song, San Francisco, CA, Claus Roehrborn, Dallas, TX
.jpg)
Ramy Said Goueli, MD, MHS
University of Texas Southwestern Medical Center
Poster Presenter(s)
Introduction: Traditional in-office uroflowmetry has been used as a diagnostic tool in lower urinary tract symptoms to guide clinical decision making but is vulnerable to several factors which may limit its validity. The “proudP” iPhone application is an audio-based uroflowmetry tool that allows for nearly unlimited flowrate recordings in the privacy of a man’s home. The objective of this study was to use the “proudP” data to assess the real-world voiding behavior in men
Methods: Men presenting to an outpatient urology clinic for lower urinary tract symptoms were given instructions to download the “proudP” applications on their smartphones for use at home. During urination, patients place their phone 3 feet above their toilet bowl and urinate directly into the center of the toilet. The application captures the sound and using a proprietary algorithm generates a voiding curve, maximal voided velocity (Qmax), average voided velocity (Qave), and volume voided (VV) (Lee et al. INJ. 2021). The data obtained was de-identified but did include date of birth. For analysis, we included men over 55 with at least 5 captured voids of 150 mL or more, collected over 2 or more days. All data is presented as mean and standard deviation, additional regression analysis was performed on Qmax to VV.
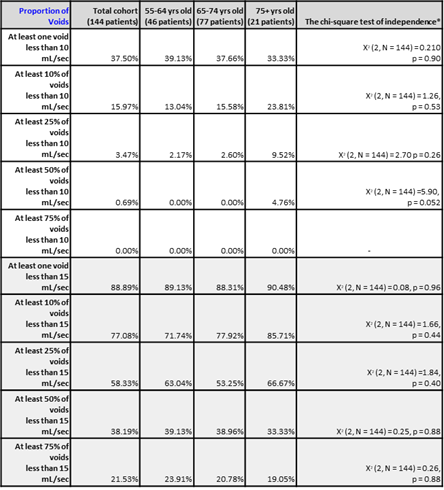
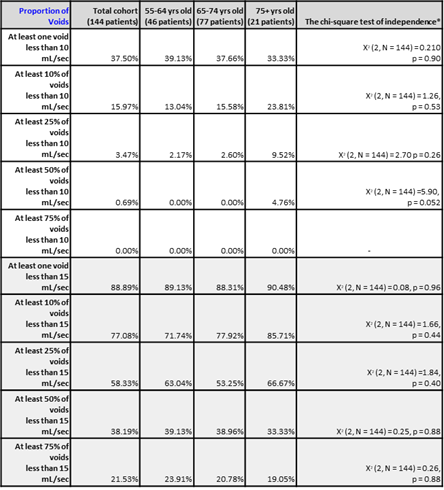
Results: Between November 2020 and October, 2021, 204 men performed at least one void on the applications, generating 10,058 individual uroflows. 144 men met our inclusion criteria, with 46 between 55-64 years old, 77 between 65-74 years old and 21 age 75 years and older. The mean age was 68.3±6.6 and each man provided an average of 58.6±86 captured voids over an average period of 20.7±23.4 days. The average VV was 244.6±109.1 and Qmax was 15.3±4.4 ml/s. There was a direct relationship between Qmax and VV that showed no significant difference between age groups. Interestingly, we found 37.5% of all men had at least one voided Qmax less than 10mL/sec, whereas 16% and 3.5% of men had at least 10% and 25% of their Qmax values <10 mL/sec, respectively. (Table 1).
Conclusions: Isolated in-office uroflowmetry may have limited generalizability as it may overestimate suspected obstruction. Aggregate flow rate data obtained from validated audio-uroflowmetry may provide a better tool for clinical stratification, measurement of therapeutic success and research.
Source of Funding: None
Methods: Men presenting to an outpatient urology clinic for lower urinary tract symptoms were given instructions to download the “proudP” applications on their smartphones for use at home. During urination, patients place their phone 3 feet above their toilet bowl and urinate directly into the center of the toilet. The application captures the sound and using a proprietary algorithm generates a voiding curve, maximal voided velocity (Qmax), average voided velocity (Qave), and volume voided (VV) (Lee et al. INJ. 2021). The data obtained was de-identified but did include date of birth. For analysis, we included men over 55 with at least 5 captured voids of 150 mL or more, collected over 2 or more days. All data is presented as mean and standard deviation, additional regression analysis was performed on Qmax to VV.
Results: Between November 2020 and October, 2021, 204 men performed at least one void on the applications, generating 10,058 individual uroflows. 144 men met our inclusion criteria, with 46 between 55-64 years old, 77 between 65-74 years old and 21 age 75 years and older. The mean age was 68.3±6.6 and each man provided an average of 58.6±86 captured voids over an average period of 20.7±23.4 days. The average VV was 244.6±109.1 and Qmax was 15.3±4.4 ml/s. There was a direct relationship between Qmax and VV that showed no significant difference between age groups. Interestingly, we found 37.5% of all men had at least one voided Qmax less than 10mL/sec, whereas 16% and 3.5% of men had at least 10% and 25% of their Qmax values <10 mL/sec, respectively. (Table 1).
Conclusions: Isolated in-office uroflowmetry may have limited generalizability as it may overestimate suspected obstruction. Aggregate flow rate data obtained from validated audio-uroflowmetry may provide a better tool for clinical stratification, measurement of therapeutic success and research.
Source of Funding: None

.jpg)
.jpg)