Back
Poster, Podium & Video Sessions
Moderated Poster
MP18: Urodynamics/Lower Urinary Tract Dysfunction/Female Pelvic Medicine: Non-neurogenic Voiding Dysfunction I
MP18-19: Urodynamics (UDS) usage for benign prostatic hyperplasia (BPH)
Friday, May 13, 2022
4:30 PM – 5:45 PM
Location: Room 222
Samantha L. Thorogood*, Tenny R. Zhang, Christina Sze, Mary O. Strasser, Gina DeMeo, Richard K. Lee, Bilal Chughtai, Alexis Te, Jim C. Hu, New York, NY

Samantha Thorogood, MD
NewYork Presbyterian/Weill Cornell Medical College
Poster Presenter(s)
Introduction: Randomized trials have not shown a benefit to UDS prior to BPH surgery; however, practice patterns associated with UDS use remain unknown. As such, we investigated factors associated with UDS use for BPH through American Board of Urology (ABU) certification/recertification case logs.
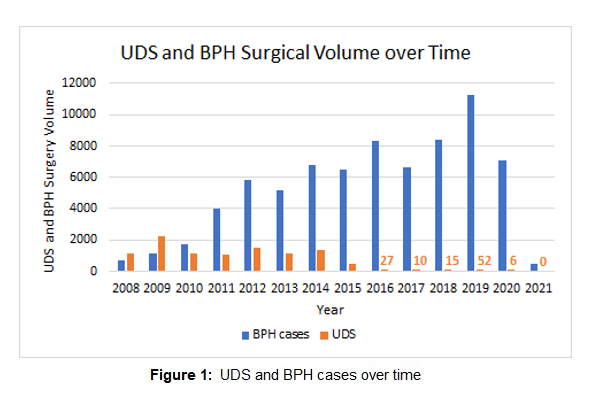
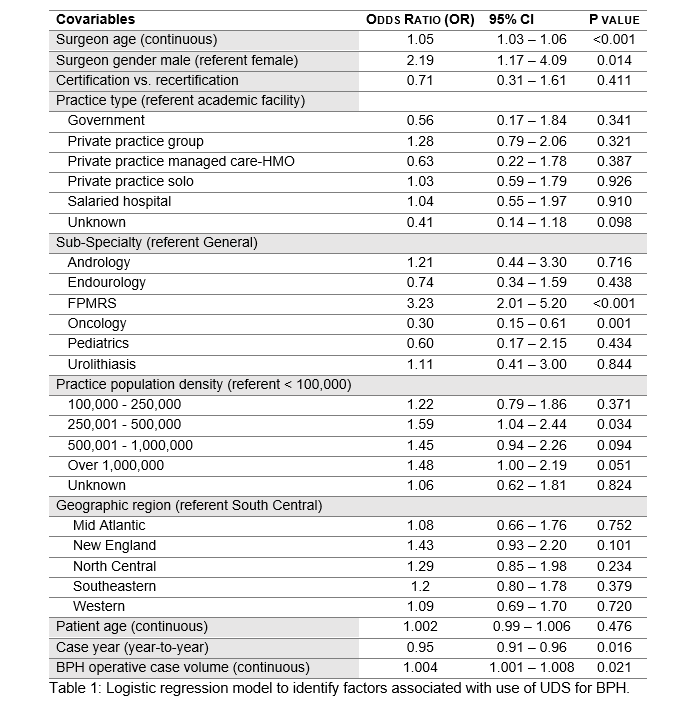
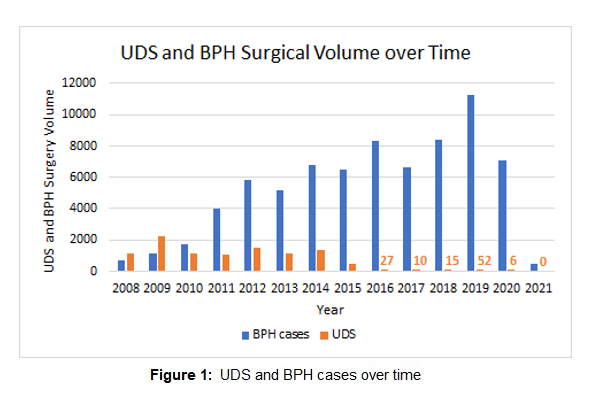
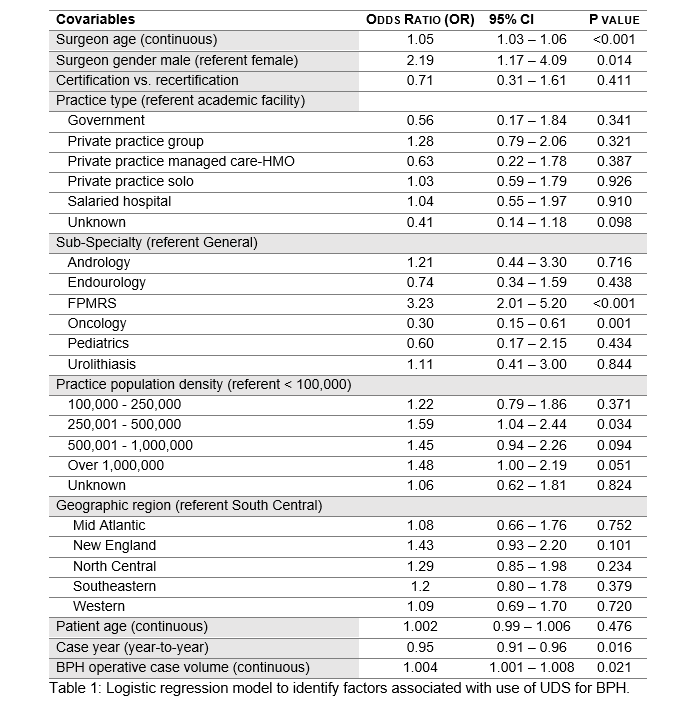
Methods: We obtained de-identified, self-reported, case logs between 2008 and 2021 from the ABU. We identified 709 urologists who performed 9,913 UDS studies linked to a BPH diagnosis. We then compared BPH urologists who did vs. did not perform UDS for a BPH indication by surgeon and patient age, gender, subspecialty, certification vs, recertification, practice type, practice population density, and geographic region. To determine factors independently associated with performing UDS for BPH, we constructed a logistic regression model with surgeon age (continuous), surgeon gender (referent female), certification vs. recertification, practice type (referent academic faculty), subspecialty (referent general), and procedure year and BPH surgical volume as continuous variables.
Results: In adjusted analysis, the odds of conducting UDS decreased annually (odds ratio [OR] 0.95/year), was higher among male (OR 2.19), older (OR 1.05), and higher volume (OR 1.004 per additional case) BPH surgeons, respectively. The odds of performing UDS was higher for female pelvic medicine and reconstructive surgery (FPMRS) specialists vs. general urologists (OR 3.23). Practice type and geographic region were not associated with the use of UDS for BPH.
Conclusions: There is significant practice pattern variation for the use of UDS. We found that the use of UDS for BPH decreased significantly over time; however older, male, and higher volume BPH surgeons and those subspecializing in FPMRS were more likely to perform UDS for BPH. Variation in care may reflect current guidelines which recommend UDS for suspected mixed etiology voiding dysfunction. More study is needed to ultimately improve concordance with high-level evidence and professional guidelines.
Source of Funding: None
Methods: We obtained de-identified, self-reported, case logs between 2008 and 2021 from the ABU. We identified 709 urologists who performed 9,913 UDS studies linked to a BPH diagnosis. We then compared BPH urologists who did vs. did not perform UDS for a BPH indication by surgeon and patient age, gender, subspecialty, certification vs, recertification, practice type, practice population density, and geographic region. To determine factors independently associated with performing UDS for BPH, we constructed a logistic regression model with surgeon age (continuous), surgeon gender (referent female), certification vs. recertification, practice type (referent academic faculty), subspecialty (referent general), and procedure year and BPH surgical volume as continuous variables.
Results: In adjusted analysis, the odds of conducting UDS decreased annually (odds ratio [OR] 0.95/year), was higher among male (OR 2.19), older (OR 1.05), and higher volume (OR 1.004 per additional case) BPH surgeons, respectively. The odds of performing UDS was higher for female pelvic medicine and reconstructive surgery (FPMRS) specialists vs. general urologists (OR 3.23). Practice type and geographic region were not associated with the use of UDS for BPH.
Conclusions: There is significant practice pattern variation for the use of UDS. We found that the use of UDS for BPH decreased significantly over time; however older, male, and higher volume BPH surgeons and those subspecializing in FPMRS were more likely to perform UDS for BPH. Variation in care may reflect current guidelines which recommend UDS for suspected mixed etiology voiding dysfunction. More study is needed to ultimately improve concordance with high-level evidence and professional guidelines.
Source of Funding: None

.jpg)
.jpg)