Back
Poster, Podium & Video Sessions
Moderated Poster
MP18: Urodynamics/Lower Urinary Tract Dysfunction/Female Pelvic Medicine: Non-neurogenic Voiding Dysfunction I
MP18-20: Evaluation Of Quality Of Life, Voiding, And Sexual Dysfunction In Patients Following Robot-Assisted Vesicovaginal Fistula Repair
Friday, May 13, 2022
4:30 PM – 5:45 PM
Location: Room 222
Pawan Kaundal, Ravimohan Mavuduru*, Girdhar Bora, Shrawan K Singh, Chandigarh , India
- RM
Poster Presenter(s)
Introduction: Robot-assisted VVF repair has the advantage of minimal surrounding tissue trauma, small cystotomy, and precise dissection, leading to a better outcome. This study aims to evaluate the quality of life, voiding, and sexual dysfunction following robot-assisted VVF repair.
Methods: Women with successful RA-VVF repair from December 2014 to June 2020 were screened using Urinary distress inventory-6(UDI-6),Incontinence impact questionnaire-7(IIQ-7), Female sexual function index(FSFI), World Health Organization quality of life(WHOQOL-BREF) questionnaires in an ambispective cohort study at 3 months of repair.Those with recto-vaginal, malignant, radiation fistulae, failed robotic repair, non-consenting, undergoing open abdominal/vaginal VVF repair and incompletely filled questionnaire were excluded.Those with urinary dysfunction were subjected to urodynamic evaluation. Appropriate Statistical test were applied using SPSS version 23.0.
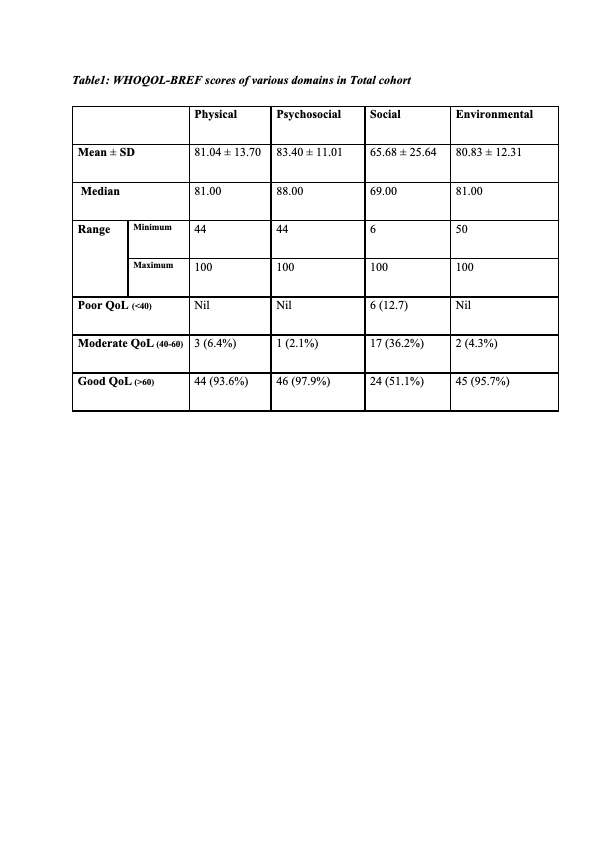
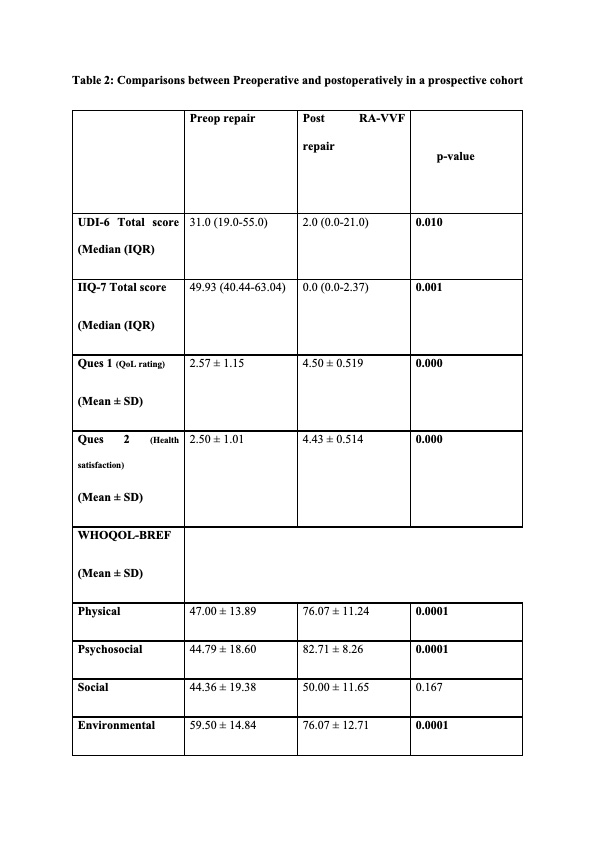
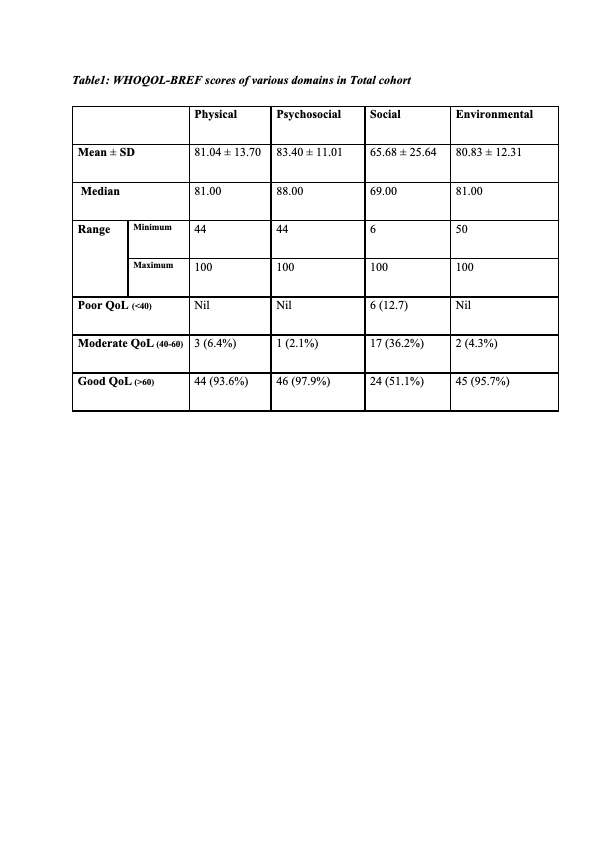
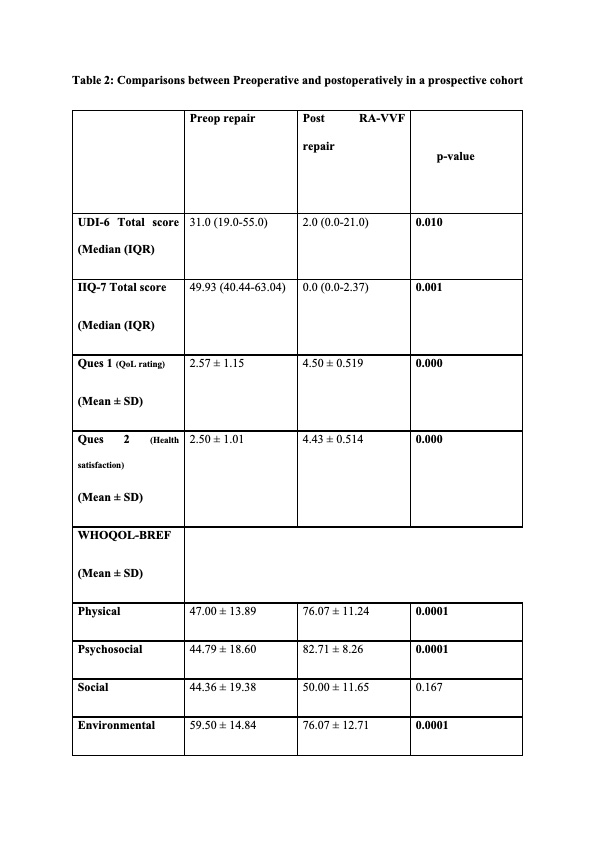
Results: 75 women underwemt RA-VVF repair. Of these 47 were enrolled(33 in retrospective and 14 in prospective cohort). Overall, 28 (60%) women had urinary complaints. The median UDI-6 score was 4 (0-100), IIQ score 0.00 (0-23). 5 (10%) women had affect on day-to-day activity and only one patient had moderate bother. However, UDS (15 women) showed normal cystometric capacity (352 ± 98.12) ml and compliance in 14 (93%) womenwith no detrusor overactivity. Mean BOOI and DCI were 11.90 ± 7.01 and 44.25 ± 8.60 respectively. 20 (43%) women were sexually active, only 2 had sexual dysfunction (FSFI score < 26.55). Quality of life was “good” to “very good” in all domains (score >90) except for the social domain (table1). Prospective cohort showed significant improvement in UDI-6 score (p < 0.05), IIQ-7 score (p < 0.5) and quality of life (p < 0.5) postoperatively.
Conclusions: RA-VVF repair results in minimal voiding dysfunction and significant improvement in overall quality of life. For sexual dysfunction assessment, longer follow-up is required.
Source of Funding: None
Methods: Women with successful RA-VVF repair from December 2014 to June 2020 were screened using Urinary distress inventory-6(UDI-6),Incontinence impact questionnaire-7(IIQ-7), Female sexual function index(FSFI), World Health Organization quality of life(WHOQOL-BREF) questionnaires in an ambispective cohort study at 3 months of repair.Those with recto-vaginal, malignant, radiation fistulae, failed robotic repair, non-consenting, undergoing open abdominal/vaginal VVF repair and incompletely filled questionnaire were excluded.Those with urinary dysfunction were subjected to urodynamic evaluation. Appropriate Statistical test were applied using SPSS version 23.0.
Results: 75 women underwemt RA-VVF repair. Of these 47 were enrolled(33 in retrospective and 14 in prospective cohort). Overall, 28 (60%) women had urinary complaints. The median UDI-6 score was 4 (0-100), IIQ score 0.00 (0-23). 5 (10%) women had affect on day-to-day activity and only one patient had moderate bother. However, UDS (15 women) showed normal cystometric capacity (352 ± 98.12) ml and compliance in 14 (93%) womenwith no detrusor overactivity. Mean BOOI and DCI were 11.90 ± 7.01 and 44.25 ± 8.60 respectively. 20 (43%) women were sexually active, only 2 had sexual dysfunction (FSFI score < 26.55). Quality of life was “good” to “very good” in all domains (score >90) except for the social domain (table1). Prospective cohort showed significant improvement in UDI-6 score (p < 0.05), IIQ-7 score (p < 0.5) and quality of life (p < 0.5) postoperatively.
Conclusions: RA-VVF repair results in minimal voiding dysfunction and significant improvement in overall quality of life. For sexual dysfunction assessment, longer follow-up is required.
Source of Funding: None

.jpg)
.jpg)