Back
Poster, Podium & Video Sessions
Moderated Poster
MP19: Education Research II
MP19-01: Racial and Ethnic Differences in Medical Student Timing and Perceived Quality of Exposure to Urology
Saturday, May 14, 2022
7:00 AM – 8:15 AM
Location: Room 228
Efe Chantal Ghanney Simons*, Natalia Garcia Peñaloza, Los Angeles, CA, Kassandra E. Zaila Ardines, Cleveland, OH, Serena Does, Utrecht, Netherlands, Samuel L. Washington III, San Francisco, CA, Megha Tandel, Clarence H. Braddock III, Los Angeles, CA, Tracy M. Downs, Charlottesville, VA, Christopher Saigal, Los Angeles , CA

Efe C. Ghanney, MD
UCLA
Poster Presenter(s)
Introduction: Little is known regarding whether exposures to urology are experienced equally by medical students of all races. To contextualize the low representation of Under-Represented in Medicine (URiM) in urology, we examine differences in timing and perceived quality of urology clinical, mentorship and research exposures for medical students across race.
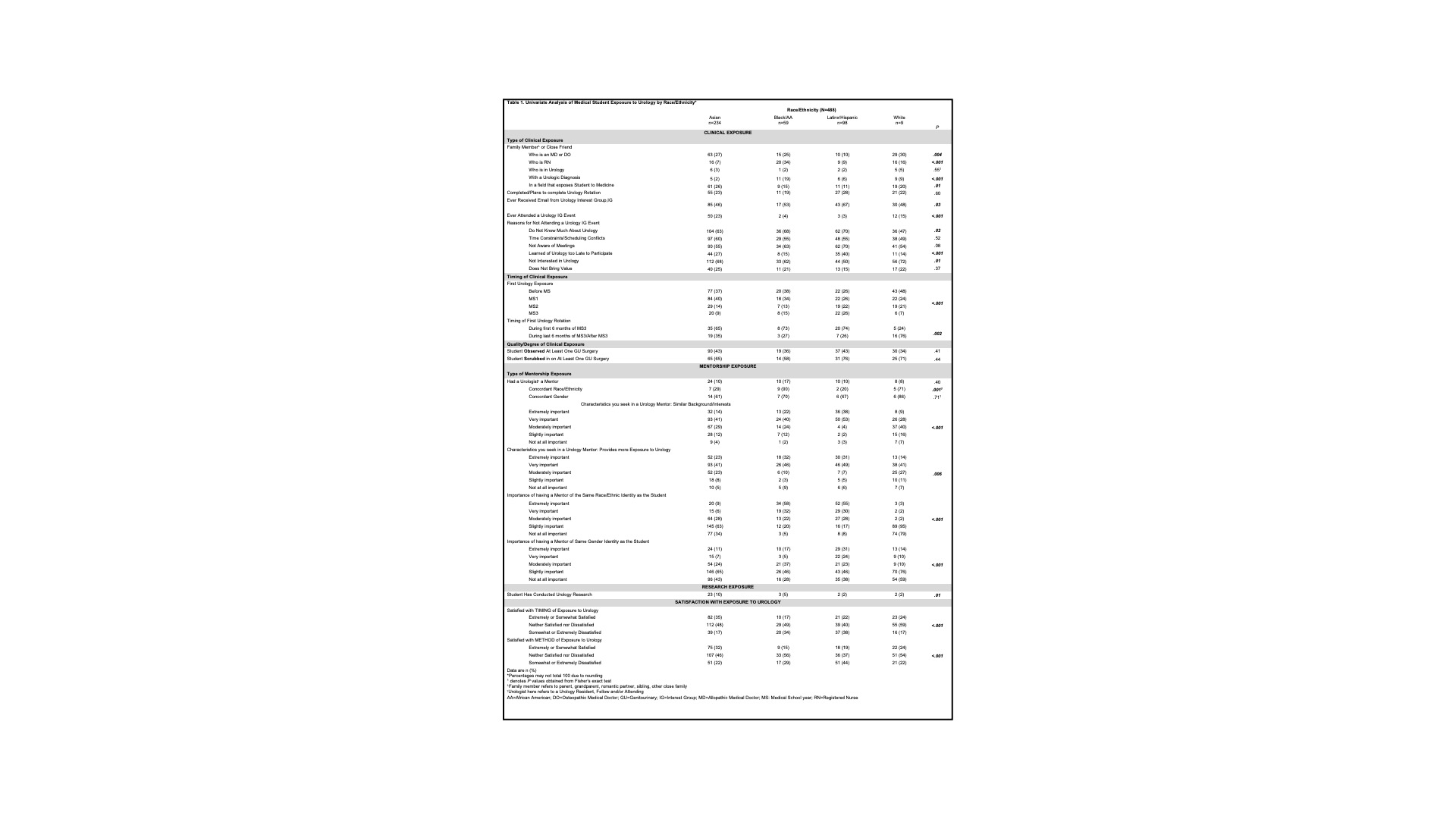
Methods: A survey was distributed to all UCLA medical students. Key dependent variables were timing of first urology exposure and perceived quality of urology exposure. Descriptive statistics and multivariate analyses were used to compare variables across race. Logistic regression was used to determine the odds of early exposure to urology across race.
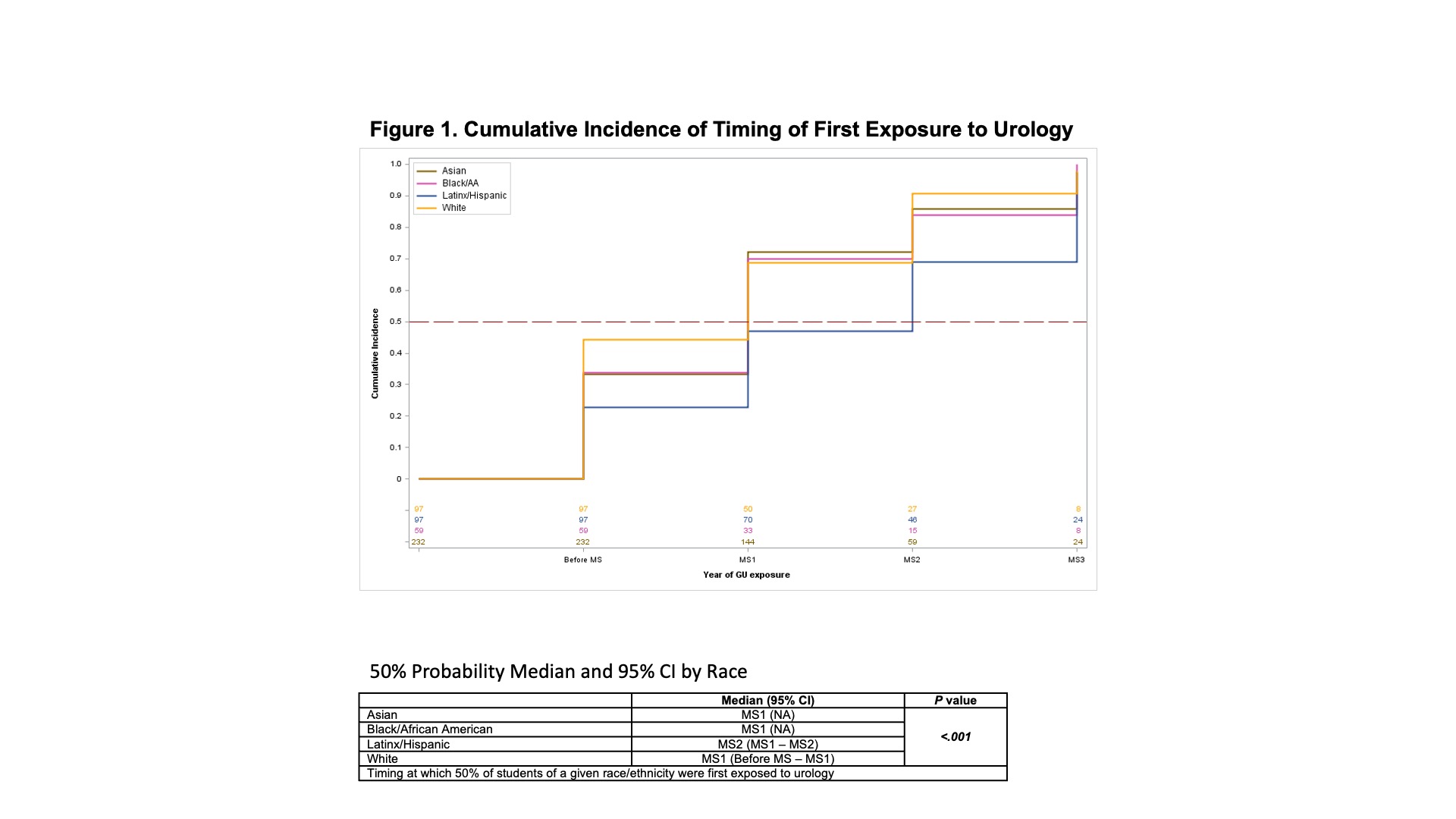
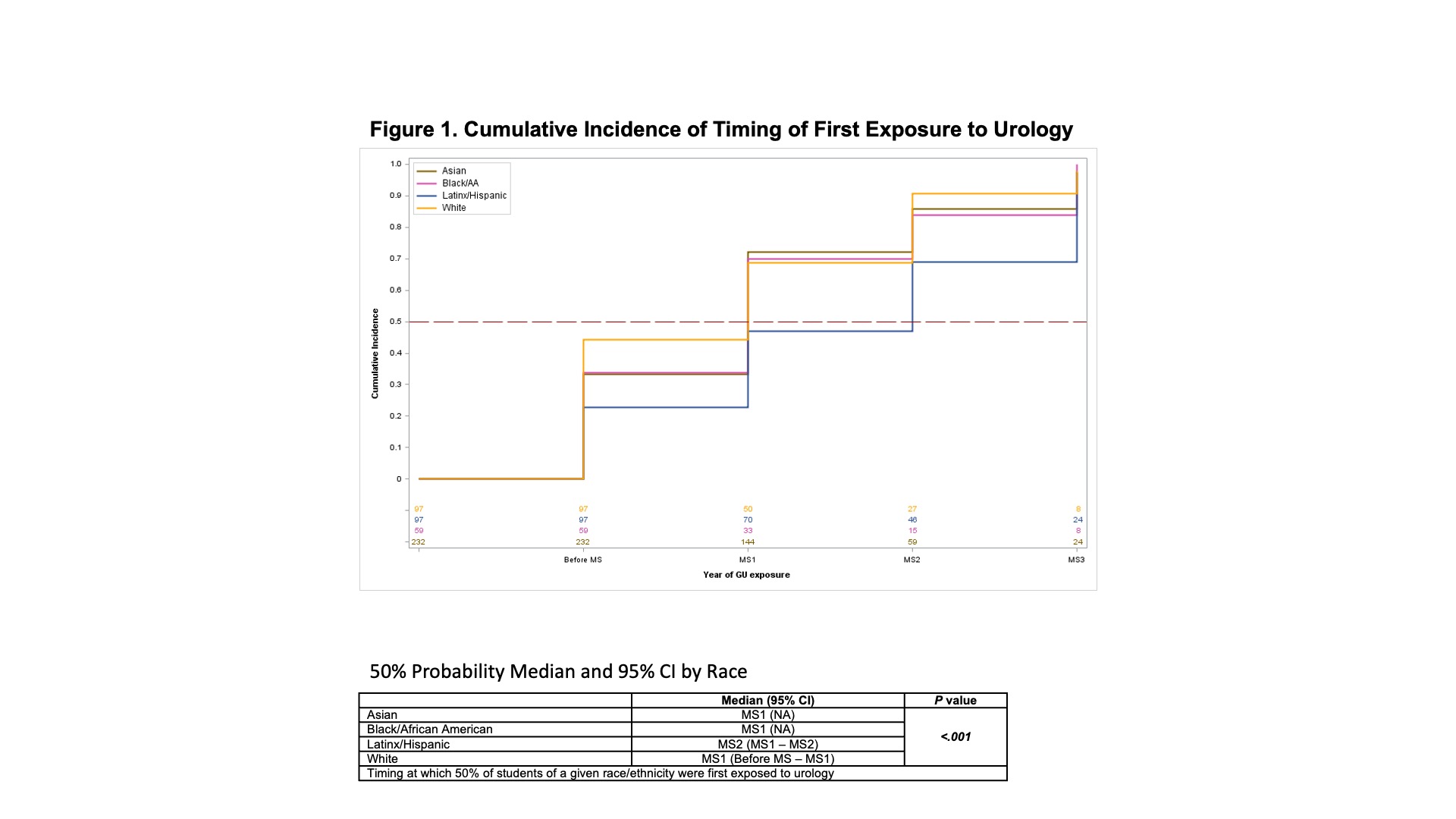
Results: Response rate was 69%. Black and Latinx students were less likely to discover urology before MS3 (P <.001). Although URiM students were more likely to recall receiving a urology interest group invitation (Asian 46%, Black 53%, Latinx 67%, White 48%, P=.03), they were less likely to attend an event (Asian 23%, Black 4%, Latinx 3% and White 15%, P<.001) despite being more likely to be interested in urology (Asian 32%, Black 38%, Latinx 50%, White 28%, P=.01). Black students were more likely to gain exposure via family/friend with a urological diagnosis. Mentor racial concordance was ‘not at all important’ for Asian (34%) and White (79%) students versus Black (58%) and Latinx (55%) students who considered it ‘extremely important’ (P <.001). Black and Latinx students were twice as dissatisfied with the timing and method of medical school exposure to urology versus their peers. There were differences across race/ethnicity for whether or not a student had engaged in urology research (Asian 10%, Black 5%, Latinx 2%, White 2%, P=.01).
Conclusions: Racial disparities exist in early exposure to urology, involvement in urology interest group events, access to research, and satisfaction with exposure to urology. Interventions addressing the timing and quality of urology exposures and mentor racial concordance may optimize recruitment of URiM students into urology.
Source of Funding: Office of the Vice Dean for Education and the Executive Director of the DGSOM AntiRacism Roadmap
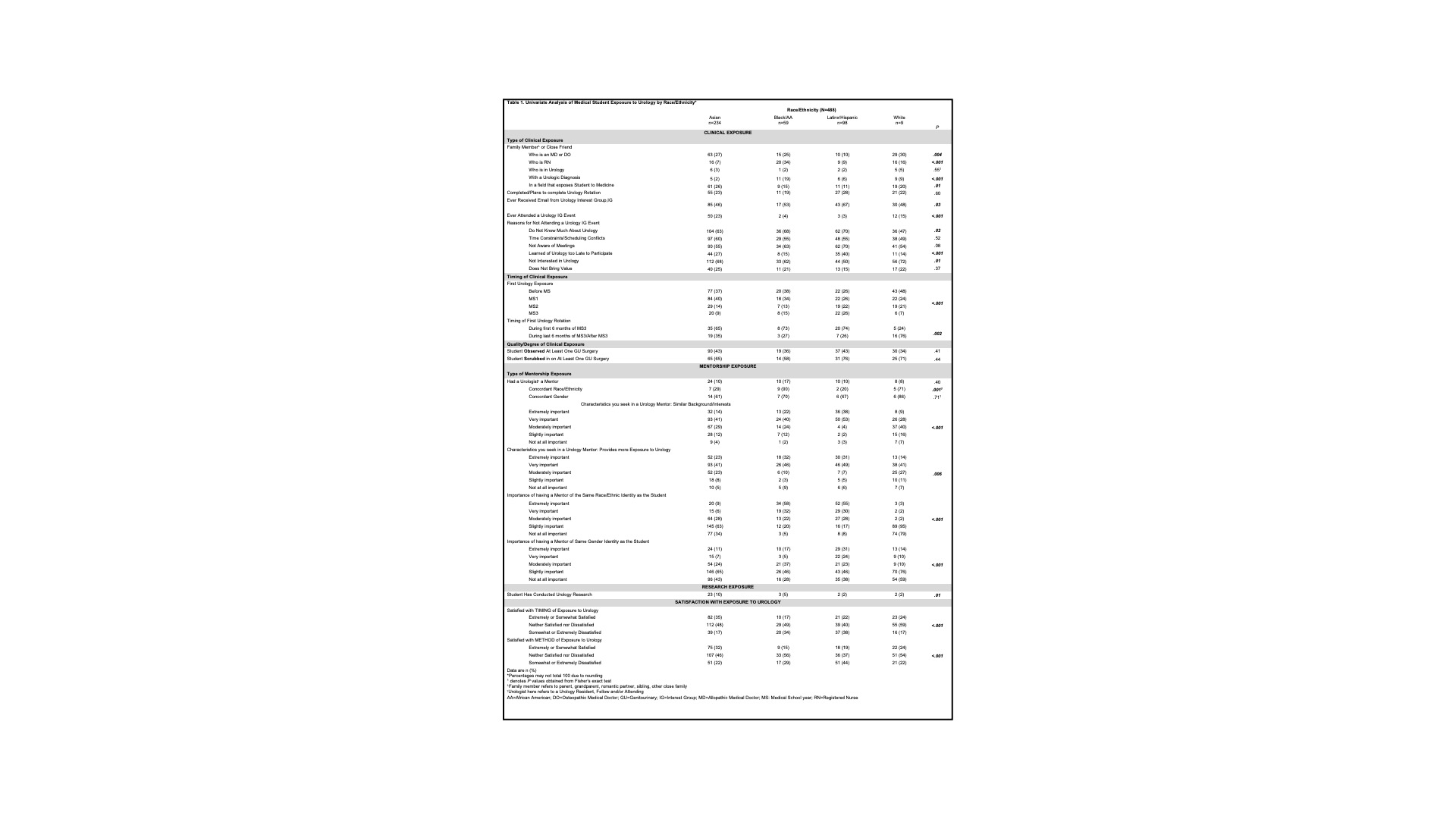
Methods: A survey was distributed to all UCLA medical students. Key dependent variables were timing of first urology exposure and perceived quality of urology exposure. Descriptive statistics and multivariate analyses were used to compare variables across race. Logistic regression was used to determine the odds of early exposure to urology across race.
Results: Response rate was 69%. Black and Latinx students were less likely to discover urology before MS3 (P <.001). Although URiM students were more likely to recall receiving a urology interest group invitation (Asian 46%, Black 53%, Latinx 67%, White 48%, P=.03), they were less likely to attend an event (Asian 23%, Black 4%, Latinx 3% and White 15%, P<.001) despite being more likely to be interested in urology (Asian 32%, Black 38%, Latinx 50%, White 28%, P=.01). Black students were more likely to gain exposure via family/friend with a urological diagnosis. Mentor racial concordance was ‘not at all important’ for Asian (34%) and White (79%) students versus Black (58%) and Latinx (55%) students who considered it ‘extremely important’ (P <.001). Black and Latinx students were twice as dissatisfied with the timing and method of medical school exposure to urology versus their peers. There were differences across race/ethnicity for whether or not a student had engaged in urology research (Asian 10%, Black 5%, Latinx 2%, White 2%, P=.01).
Conclusions: Racial disparities exist in early exposure to urology, involvement in urology interest group events, access to research, and satisfaction with exposure to urology. Interventions addressing the timing and quality of urology exposures and mentor racial concordance may optimize recruitment of URiM students into urology.
Source of Funding: Office of the Vice Dean for Education and the Executive Director of the DGSOM AntiRacism Roadmap

.jpg)
.jpg)