Back
Poster, Podium & Video Sessions
Best Poster Award
MP19: Education Research II
MP19-03: Trends in Race and Ethnicity Among Applicants to US Urology Residency Programs
Saturday, May 14, 2022
7:00 AM – 8:15 AM
Location: Room 228
Efe Chantal Ghanney Simons*, Parris A. Diaz, Los Angeles, CA, Rebecca Takele, Blacksburg, VA, Serena Does, Utrecht, Netherlands, Samuel L. Washington III, San Francisco, CA, Benjamin N. Breyer, San Francisco , CA, Holly Wilhalme, Los Angeles, CA, Tracy M. Downs, Charlottesville, VA, Christopher Saigal, Los Angeles , CA

Efe C. Ghanney, MD
UCLA
Poster Presenter(s)
Introduction: Despite an increase in the racial and ethnic diversity of the US population over the past decade, the proportion of Under-Represented in Medicine (URiM) urologists has remained stagnant. This current work disaggregates urology residency applicant demographic data by race and ethnicity. Secondly, we determine if there are differences across race/ethnicity in outcome measures related to the Urology Match.
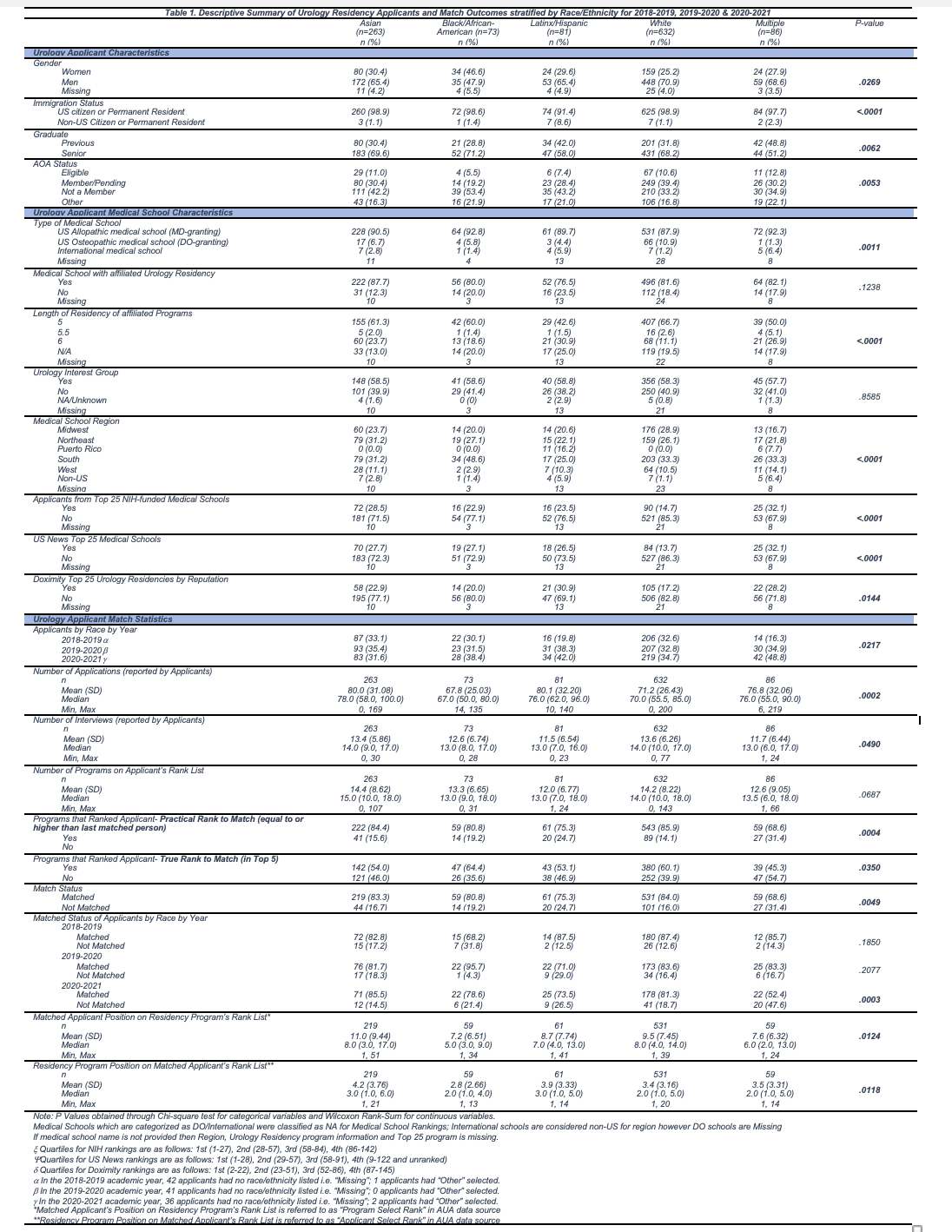
Methods: Urology residency applicant data for 2018-2019 to 2020-2021 was provided by the Society of Academic Urologists through the American Urological Association. The self-reported racial/ethnic groups examined were Asian, Black, Latinx, White and Multiple Race. Key dependent variables were (i) number of applications, interviews and programs on the applicant's rank list, (ii) being ranked to match i.e. in top 5 spot on program's rank list vs. ranked higher than the last matched person, and (iii) match status, applicant position on program's rank list and vice versa. Chi square and Wilcoxon Rank-Sum tests were performed to assess for differences across race/ethnicity for categorical and continuous variables.
Results: Latinx applicants were least likely to be a senior when applying (Asian 70%, Black 71%, Latinx 58%, White 68% P=.02). Black applicants are least likely to be AOA members (Asian 30%, Black 19%, Latinx 28%, White 39% P=.01).
URiM applicants are less likely to be DO students (Asian 7%, Black 6%, Latinx 4%, White 11% P<.01) and there is no difference across race for whether an applicant attends a medical school without an affiliated urology residency. White applicants are least likely to come from a top 25 medical school when ranked by US News & World Report, NIH-funding or Doximity Residency Reputation.
URiM applicants have fewer of interviews (Mean: Asian 13.4, Black 12.6, Latinx 11.5, White 13.6 P=.049). While Black and Latinx applicants are the most and least likely to be ranked top 5 by a program (Asian 54%, Black 64%, Latinx 53% and White 60% P=.04), fewer URiM applicants are ranked higher than the last matched person (Asian 84%, Black 81%, Latinx 75% and White 86% P<.001), therefore fewer URiM successfully match (Asian 83%, Black 81%, Latinx 75% and White 84% P<.001).
Conclusions: Understanding the urology residency match population can provide the foundation for data-driven interventions to diversify the field of urology.
Source of Funding: None
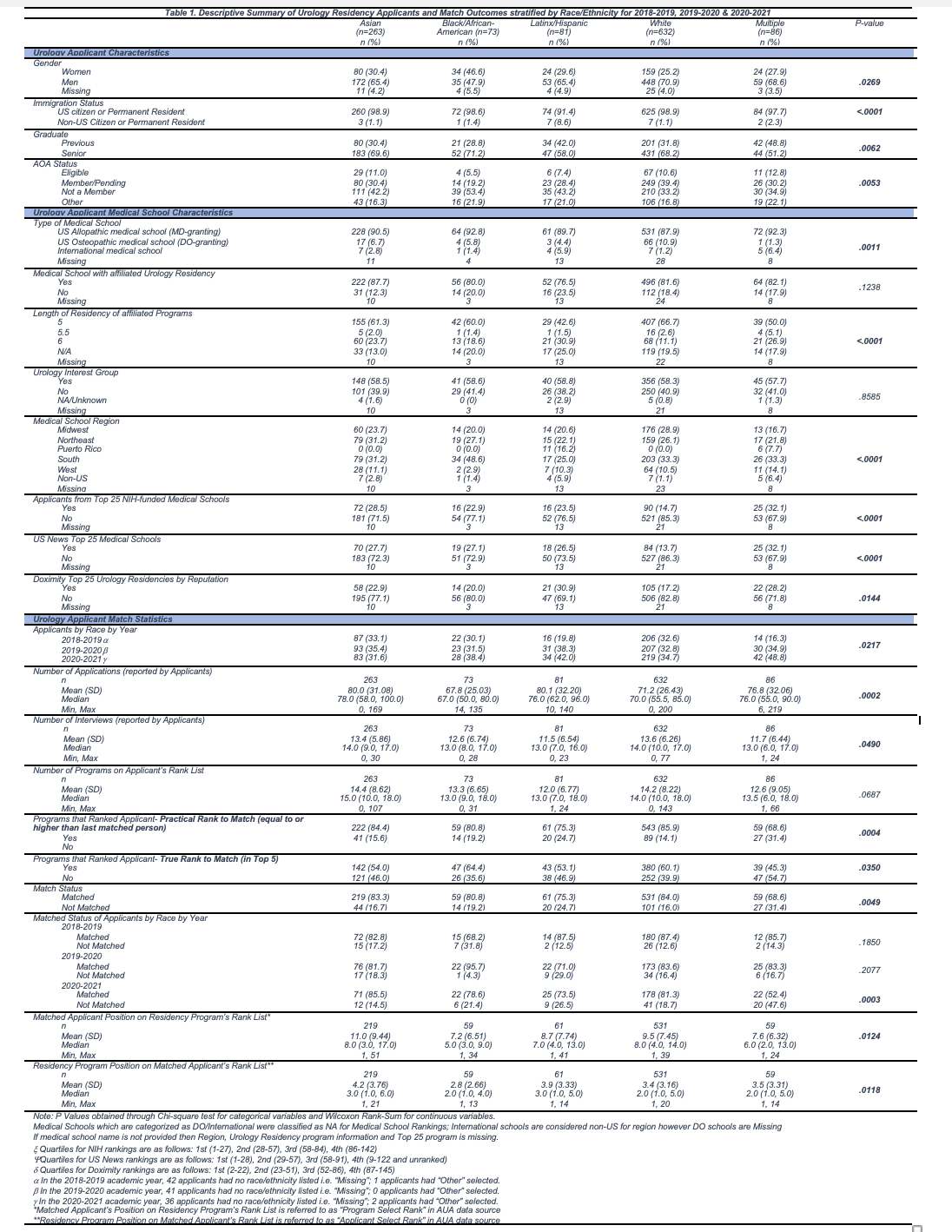
Methods: Urology residency applicant data for 2018-2019 to 2020-2021 was provided by the Society of Academic Urologists through the American Urological Association. The self-reported racial/ethnic groups examined were Asian, Black, Latinx, White and Multiple Race. Key dependent variables were (i) number of applications, interviews and programs on the applicant's rank list, (ii) being ranked to match i.e. in top 5 spot on program's rank list vs. ranked higher than the last matched person, and (iii) match status, applicant position on program's rank list and vice versa. Chi square and Wilcoxon Rank-Sum tests were performed to assess for differences across race/ethnicity for categorical and continuous variables.
Results: Latinx applicants were least likely to be a senior when applying (Asian 70%, Black 71%, Latinx 58%, White 68% P=.02). Black applicants are least likely to be AOA members (Asian 30%, Black 19%, Latinx 28%, White 39% P=.01).
URiM applicants are less likely to be DO students (Asian 7%, Black 6%, Latinx 4%, White 11% P<.01) and there is no difference across race for whether an applicant attends a medical school without an affiliated urology residency. White applicants are least likely to come from a top 25 medical school when ranked by US News & World Report, NIH-funding or Doximity Residency Reputation.
URiM applicants have fewer of interviews (Mean: Asian 13.4, Black 12.6, Latinx 11.5, White 13.6 P=.049). While Black and Latinx applicants are the most and least likely to be ranked top 5 by a program (Asian 54%, Black 64%, Latinx 53% and White 60% P=.04), fewer URiM applicants are ranked higher than the last matched person (Asian 84%, Black 81%, Latinx 75% and White 86% P<.001), therefore fewer URiM successfully match (Asian 83%, Black 81%, Latinx 75% and White 84% P<.001).
Conclusions: Understanding the urology residency match population can provide the foundation for data-driven interventions to diversify the field of urology.
Source of Funding: None

.jpg)
.jpg)