Back
Poster, Podium & Video Sessions
Moderated Poster
MP19: Education Research II
MP19-05: Landscape Analysis of the Use of Holistic Review in the Urology Residency Match Process
Saturday, May 14, 2022
7:00 AM – 8:15 AM
Location: Room 228
Efe Chantal Ghanney Simons*, Parris A. Diaz, Los Angeles, CA, Rebecca Takele, Blacksburg, VA, Serena Does, Utrecht, Netherlands, Nicholas J. Jackson, Los Angeles, CA, Samuel L. Washington III, San Francisco, CA, Benjamin N. Breyer, San Francisco , CA, Tracy M. Downs, Charlottesville, VA, Christopher Saigal, Los Angeles , CA

Efe C. Ghanney, MD
UCLA
Poster Presenter(s)
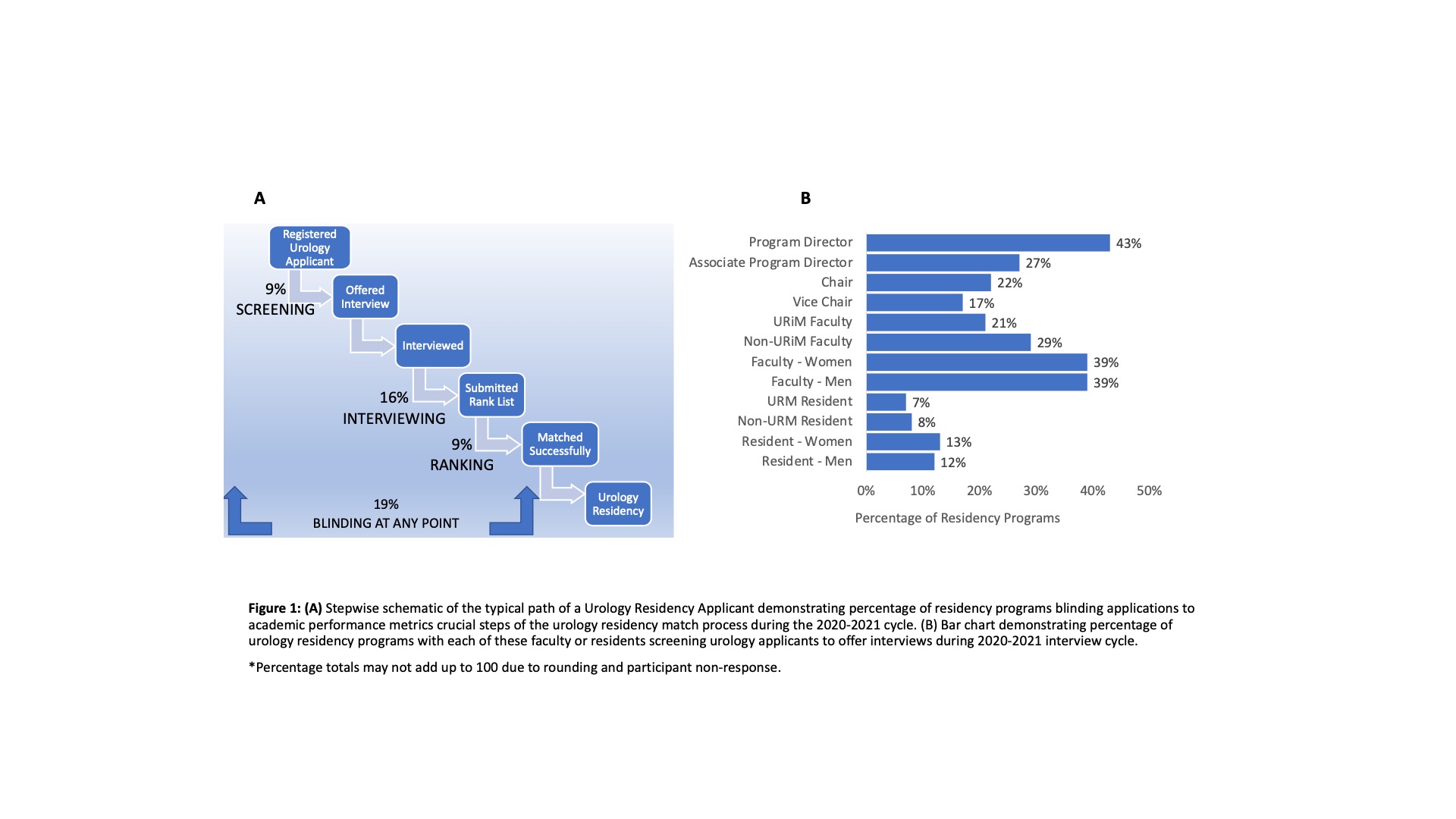
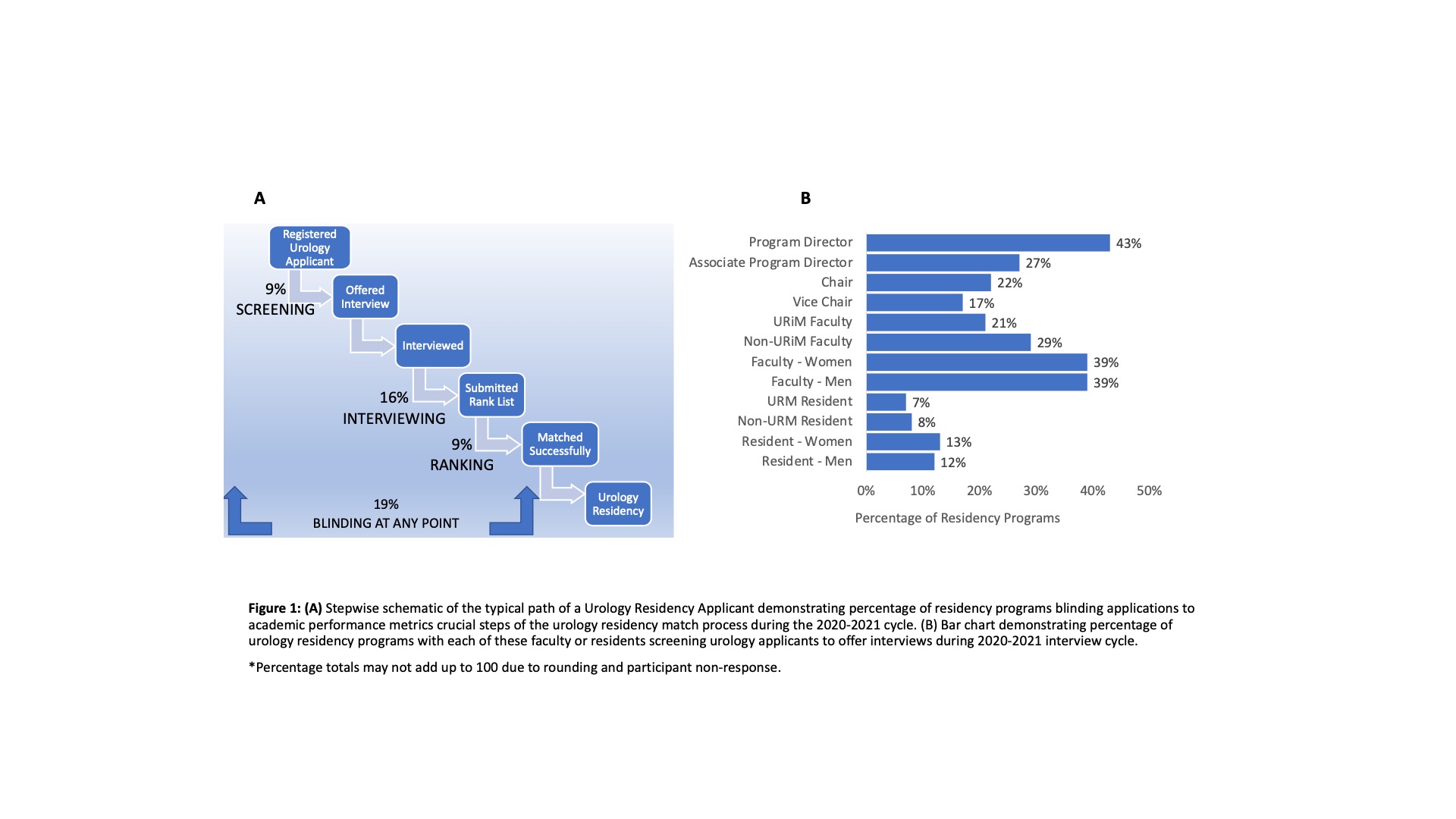
Introduction: The Association of American Medical Colleges calls on residency program leadership to adopt Holistic Review in the selection of applicants when screening, interviewing and creating rank order lists however the method of implementation is at the discretion of individual programs. Other specialties have employed blinding recruiters to standardized and increasing the diversity of their recruitment teams. In this work, we aimed to first describe the use of blinding of academic performance metrics at each stage of the urology match process and second, to describe the diversity of individuals involved in the screening of applicants to invite for interview during the Urology Residency Match process.
Methods: A cross-sectional survey of program leadership at the 144 accredited urology residency programs in the US was distributed January 29, 2021 to March 4, 2021 via the Society of Academic Urologists mailing list. Descriptive statistics were performed to determine the proportion of urology residency programs blinding academic performance metrics including USMLE Step 1 and 2 scores, GPA, class rank, honors during screening, interviewing and ranking of urology applicants.
Results: We received responses from 130 urology (associate) program directors representing 112 programs (112/144 = 78%). In the 2020-2021 urology residency application cycle, 9%, 16% and 9% of urology residency programs blinded their recruitment team to academic performance metrics at the screening, interviewing and ranking steps respectively. An equal proportion of programs report having a female faculty screen applications as those that report having male faculty (39%). Fewer programs report having Under-Represented in Medicine (URiM) faculty screen applications (21%) vs those that report non-URiM faculty involvement in screening (27%). Few programs report having resident involvement in screening and only 7% of programs include URiM residents.
Conclusions: A minority of urology residency programs currently employ blinding of scores as part of Holistic review. Fewer programs involve URiM faculty or URiM residents in the screening process. An understanding of the current practices of residency programs can inform strategies for optimizing equity, diversity and inclusion in the urology match process.
Source of Funding: None
Methods: A cross-sectional survey of program leadership at the 144 accredited urology residency programs in the US was distributed January 29, 2021 to March 4, 2021 via the Society of Academic Urologists mailing list. Descriptive statistics were performed to determine the proportion of urology residency programs blinding academic performance metrics including USMLE Step 1 and 2 scores, GPA, class rank, honors during screening, interviewing and ranking of urology applicants.
Results: We received responses from 130 urology (associate) program directors representing 112 programs (112/144 = 78%). In the 2020-2021 urology residency application cycle, 9%, 16% and 9% of urology residency programs blinded their recruitment team to academic performance metrics at the screening, interviewing and ranking steps respectively. An equal proportion of programs report having a female faculty screen applications as those that report having male faculty (39%). Fewer programs report having Under-Represented in Medicine (URiM) faculty screen applications (21%) vs those that report non-URiM faculty involvement in screening (27%). Few programs report having resident involvement in screening and only 7% of programs include URiM residents.
Conclusions: A minority of urology residency programs currently employ blinding of scores as part of Holistic review. Fewer programs involve URiM faculty or URiM residents in the screening process. An understanding of the current practices of residency programs can inform strategies for optimizing equity, diversity and inclusion in the urology match process.
Source of Funding: None

.jpg)
.jpg)