Back
Poster, Podium & Video Sessions
Moderated Poster
MP19: Education Research II
MP19-10: Determining the Effectiveness of a Deliberate Practice Training Platform in a Virtual Reality (VR) Urethrovesical Anastomosis Curriculum
Saturday, May 14, 2022
7:00 AM – 8:15 AM
Location: Room 228
Kit Yuen*, Alexis Steinmetz, Rachel Melnyk, Nathan Schuler, Galen Cheng, Dennis Phan, Ahmed Ghazi, Rochester, NY

Kit Yuen, MD, MA
University of Rochester Medical Center
Poster Presenter(s)
Introduction: Effective and independent VR training is essential to optimize robotic training. Our study sought to evaluate a deliberate practice (DP) framework incorporated into a VR urethrovesical anastomosis (UVA) curriculum to improve skill transference.
Methods: Ten medical students with no robotic surgery experience were recruited for a 4-phase curriculum. Phase 1 Pre-Learning – 7 basic VR exercises on SimNow DaVinci Simulator, completed to competency standards (>90%). Phase 2 Pre-test – UVA on a validated realistic hydrogel model and a blinded reviewers graded RACE scores. Phase 3 Training – Trainees randomly allocated to the control group (n=4) performed repetitions of the VR procedural task “Guided UVA” and received a report that identified deficient areas after each VR attempt. The DP group (n=6) was additionally assigned specific basic modules targeting these deficiencies to be completed between UVA VR attempts (Figure 1). Both groups repeated the VR UVA to proficiency (2 SEM from expert mean). Phase 4 Post-test – A second hydrogel model was performed and scored. Performance differences between pre- and post-test established the effect of the VR training curriculum.
Results: DP group reached expert benchmarks in 7.5 UVA simulation attempts with 4.9 hours of total sim time while the control group averaged 8.75 attempts over 2.8 hours. The DP group progressed faster to proficiency than the control group in the subcategories of needle handling (3.5 vs 6.75 attempts) and complications (3.5 vs 6.25) but progressed similarly in economy benchmarks (7 vs 7.25). This translated into significant increases in pre-post hydrogel model performance in the DP group with RACE scores of 13.5 to 23 (p < 0.001) and every subscore except tissue approximation. The control group did not experience a significant change in pre-post RACE scores (14.5 to 21; p=0.08) or any subscores.
Conclusions: A focused approach addressing specific skill deficiencies using the DP framework resulted in significant improvement in hydrogel UVA performance. This suggests that surgical skills acquired during DP are not task specific and improve both overall skills acquisition and transfer to performance improvement on a realistic hydrogel model.
Source of Funding: NA
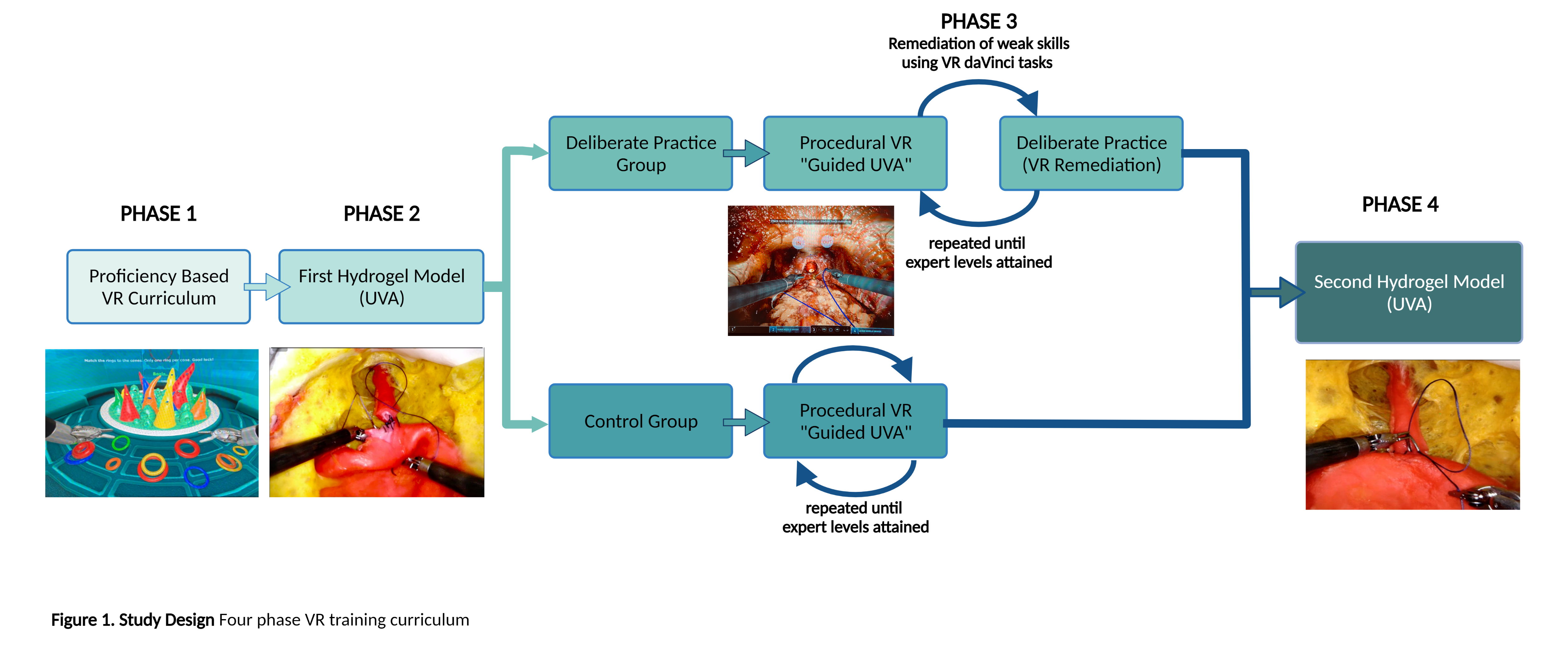
Methods: Ten medical students with no robotic surgery experience were recruited for a 4-phase curriculum. Phase 1 Pre-Learning – 7 basic VR exercises on SimNow DaVinci Simulator, completed to competency standards (>90%). Phase 2 Pre-test – UVA on a validated realistic hydrogel model and a blinded reviewers graded RACE scores. Phase 3 Training – Trainees randomly allocated to the control group (n=4) performed repetitions of the VR procedural task “Guided UVA” and received a report that identified deficient areas after each VR attempt. The DP group (n=6) was additionally assigned specific basic modules targeting these deficiencies to be completed between UVA VR attempts (Figure 1). Both groups repeated the VR UVA to proficiency (2 SEM from expert mean). Phase 4 Post-test – A second hydrogel model was performed and scored. Performance differences between pre- and post-test established the effect of the VR training curriculum.
Results: DP group reached expert benchmarks in 7.5 UVA simulation attempts with 4.9 hours of total sim time while the control group averaged 8.75 attempts over 2.8 hours. The DP group progressed faster to proficiency than the control group in the subcategories of needle handling (3.5 vs 6.75 attempts) and complications (3.5 vs 6.25) but progressed similarly in economy benchmarks (7 vs 7.25). This translated into significant increases in pre-post hydrogel model performance in the DP group with RACE scores of 13.5 to 23 (p < 0.001) and every subscore except tissue approximation. The control group did not experience a significant change in pre-post RACE scores (14.5 to 21; p=0.08) or any subscores.
Conclusions: A focused approach addressing specific skill deficiencies using the DP framework resulted in significant improvement in hydrogel UVA performance. This suggests that surgical skills acquired during DP are not task specific and improve both overall skills acquisition and transfer to performance improvement on a realistic hydrogel model.
Source of Funding: NA

.jpg)
.jpg)