Back
Poster, Podium & Video Sessions
Moderated Poster
MP20: Trauma/Reconstruction/Diversion: External Genitalia Reconstruction and Urotrauma (including transgender surgery) I
MP20-13: Quantifying Time To Orgasm After Gender Affirming Vaginoplasty
Saturday, May 14, 2022
7:00 AM – 8:15 AM
Location: Room 225
Gaines Blasdel*, Elijah Castle, New York, NY, Carmen Kloer, Durham, NC, Augustus Parker, Rachel Bluebond-Langner, Lee Zhao, New York, NY

Gaines Blasdel
Research Associate
New York University Langone Health
Poster Presenter(s)
Introduction: Many transgender and nonbinary (henceforth, “trans”) patients have goals related to sexual health when seeking gender affirming vaginoplasty, and previous investigations have only studied ability to orgasm at cross-sectional timepoints. Our aim is to quantify the time to orgasm postoperative primary robotic peritoneal gender affirming vaginoplasty and describe potential correlative factors, including pre-operative orgasm to better inform preoperative counseling.
Methods: Retrospective chart review was utilized to extract factors thought to influence pre- and post-operative orgasm in patients undergoing robotic peritoneal flap vaginoplasty. Mean days to orgasm plus one standard deviation above that mean was used to define time at which patients would be considered anorgasmic.
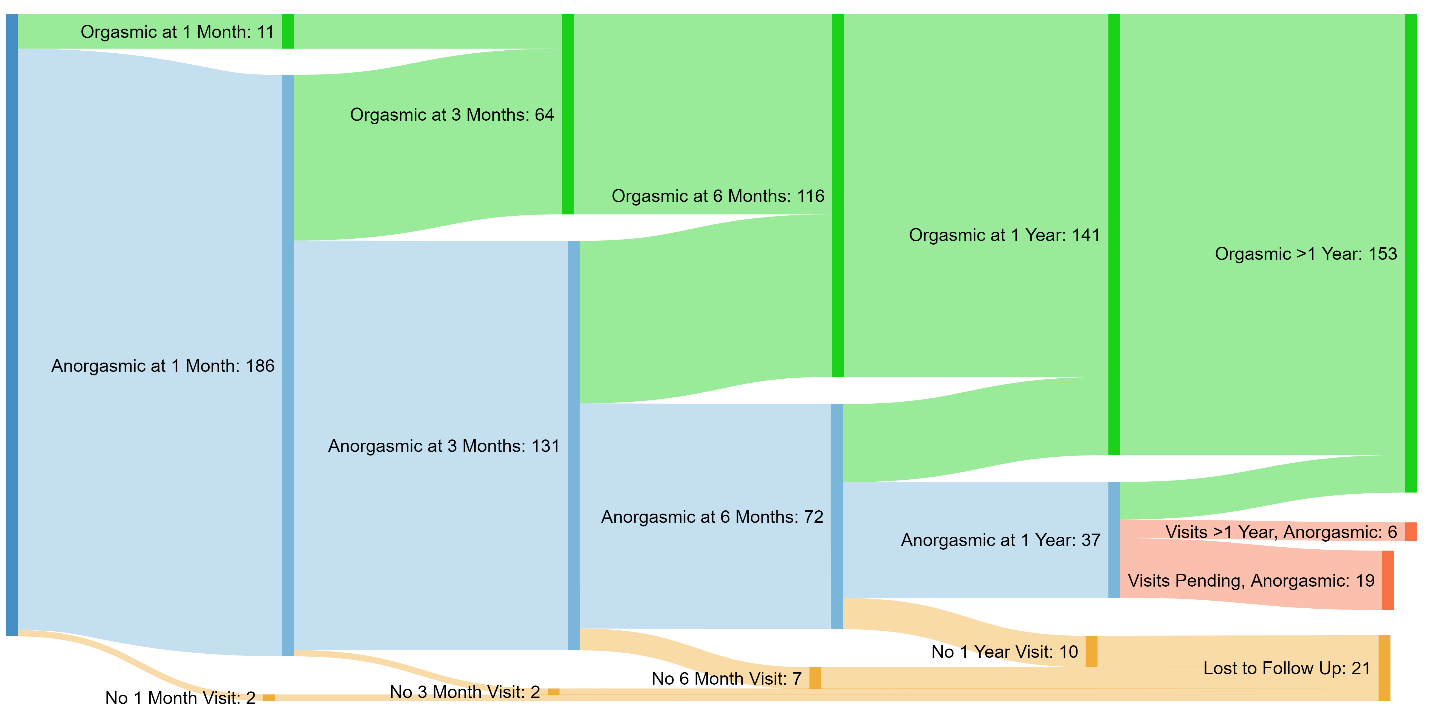
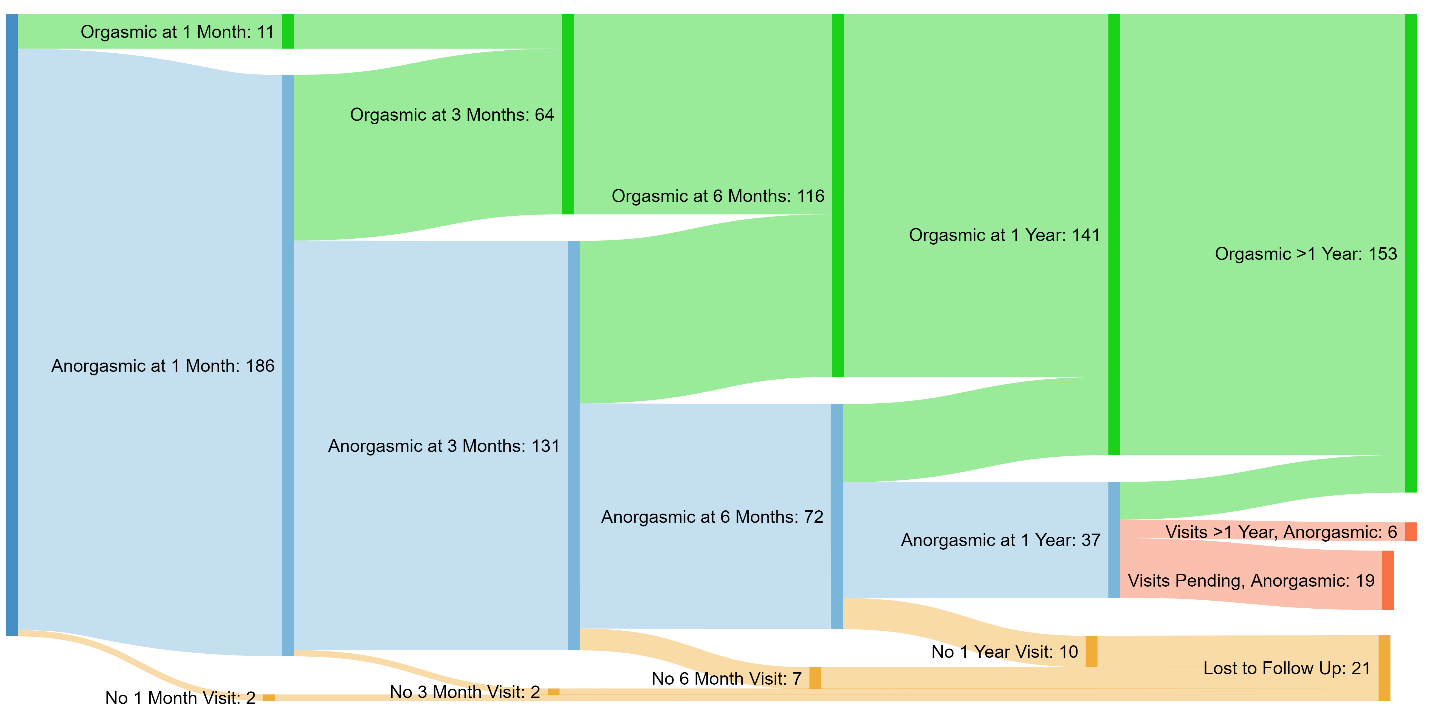
Results: A total of 199 trans patients underwent surgery from September 2017 to August 2020. Median time to orgasm was 180 days. 178 patients had completed one year of follow up or greater, and of these patients, 153 (86%) were orgasmic and 25 patients (14%) were not (Figure 1). Difficulty in pre-operative orgasm was correlated only with older age (median age 45.9 years versus 31.7, p = .03). Post-operative orgasm was not significantly correlated with pre-operative orgasm. The only factor related to post-operative orgasm was smoking history: 12 of 55 patients (21.8%) who had a positive smoking history and sufficient follow up reported anorgasmia (p-value 0.046).
Conclusions: Preoperative difficulty with orgasm appears to be treated with gender affirming vaginoplasty, conferring similar post-surgical orgasm rates to those who struggled with orgasm before surgery. Smoking had a negative impact on post-operative orgasm recovery despite negative cotinine test prior to surgery, signaling that prolonged smoking cessation may improve orgasmic outcomes, or that underlying exposures correlated with smoking may be the true causal factor inhibiting recovery of orgasm. The majority of patients were orgasmic at their six month follow up appointment, however patients became newly orgasmic in appreciable numbers more than one year after surgery. Interventions for anorgasmic patients include testosterone replacement, pelvic floor physical therapy, and psychotherapy.
Source of Funding: None.
Methods: Retrospective chart review was utilized to extract factors thought to influence pre- and post-operative orgasm in patients undergoing robotic peritoneal flap vaginoplasty. Mean days to orgasm plus one standard deviation above that mean was used to define time at which patients would be considered anorgasmic.
Results: A total of 199 trans patients underwent surgery from September 2017 to August 2020. Median time to orgasm was 180 days. 178 patients had completed one year of follow up or greater, and of these patients, 153 (86%) were orgasmic and 25 patients (14%) were not (Figure 1). Difficulty in pre-operative orgasm was correlated only with older age (median age 45.9 years versus 31.7, p = .03). Post-operative orgasm was not significantly correlated with pre-operative orgasm. The only factor related to post-operative orgasm was smoking history: 12 of 55 patients (21.8%) who had a positive smoking history and sufficient follow up reported anorgasmia (p-value 0.046).
Conclusions: Preoperative difficulty with orgasm appears to be treated with gender affirming vaginoplasty, conferring similar post-surgical orgasm rates to those who struggled with orgasm before surgery. Smoking had a negative impact on post-operative orgasm recovery despite negative cotinine test prior to surgery, signaling that prolonged smoking cessation may improve orgasmic outcomes, or that underlying exposures correlated with smoking may be the true causal factor inhibiting recovery of orgasm. The majority of patients were orgasmic at their six month follow up appointment, however patients became newly orgasmic in appreciable numbers more than one year after surgery. Interventions for anorgasmic patients include testosterone replacement, pelvic floor physical therapy, and psychotherapy.
Source of Funding: None.

.jpg)
.jpg)