Back
Poster, Podium & Video Sessions
Moderated Poster
MP21: Sexual Function/Dysfunction: Evaluation I
MP21-14: U-shaped Association Between Secondary Hypogonadism and Body Mass Index: A Retrospective Analysis of Men with Testosterone Deficiency
Saturday, May 14, 2022
7:00 AM – 8:15 AM
Location: Room 222
Aaron A. Gurayah*, Miami, FL, John M. Masterson, Los Angeles, CA, Atil Y. Kargi, Ranjith Ramasamy, Miami, FL

Aaron Adrian Gurayah, BA
University of Miami Miller School of Medicine
Poster Presenter(s)
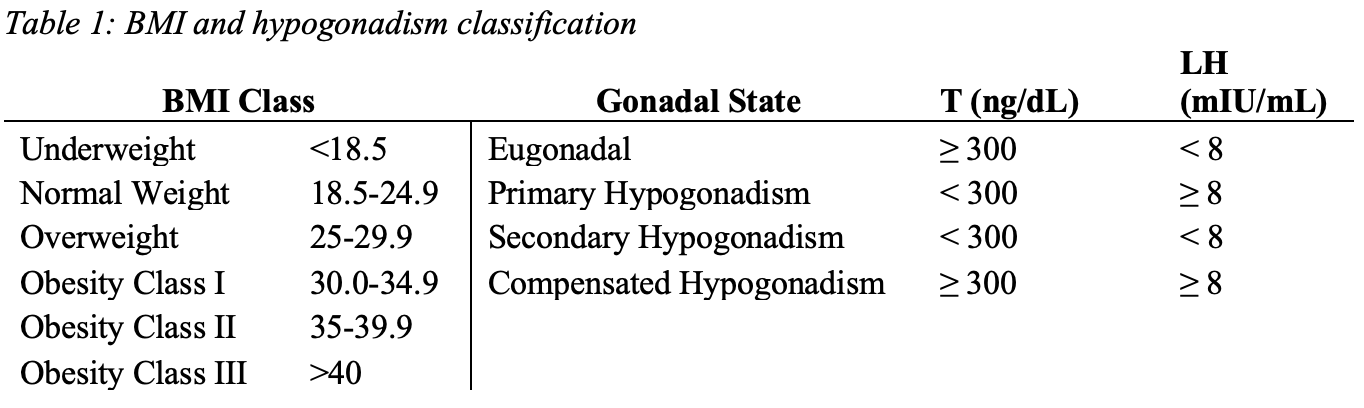
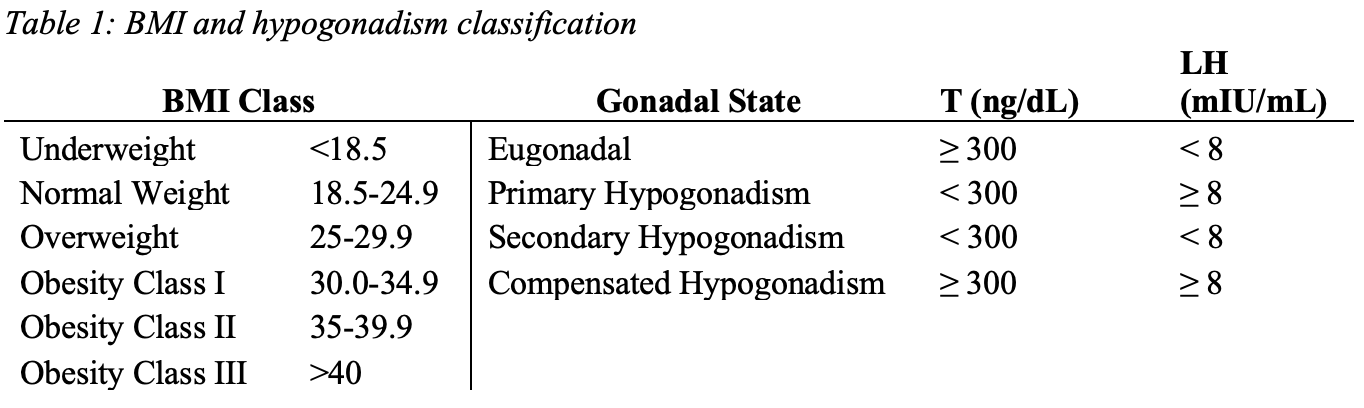
Introduction: The prevalence of both obesity and hypogonadism in the United States has increased over the past two decades. While prior studies have shown an association between obesity and secondary hypogonadism—men with low testosterone (T) and luteinizing hormone (LH)—few have used a large enough sample size to determine prevalence at each body mass index (BMI) class. We hypothesized that secondary hypogonadism becomes more prevalent with increasing BMI. Our study aimed to compare the prevalence of secondary hypogonadism among BMI classes.
Methods: We constructed a retrospective database with men who had their BMI, morning T and LH levels measured during a visit to a urology clinic at a tertiary academic medical center between 2011-2020. Men previously on testosterone replacement therapy (TRT), Clomiphene, or Anastrozole were excluded. Chi-squared analysis was conducted in R (4.1.1).
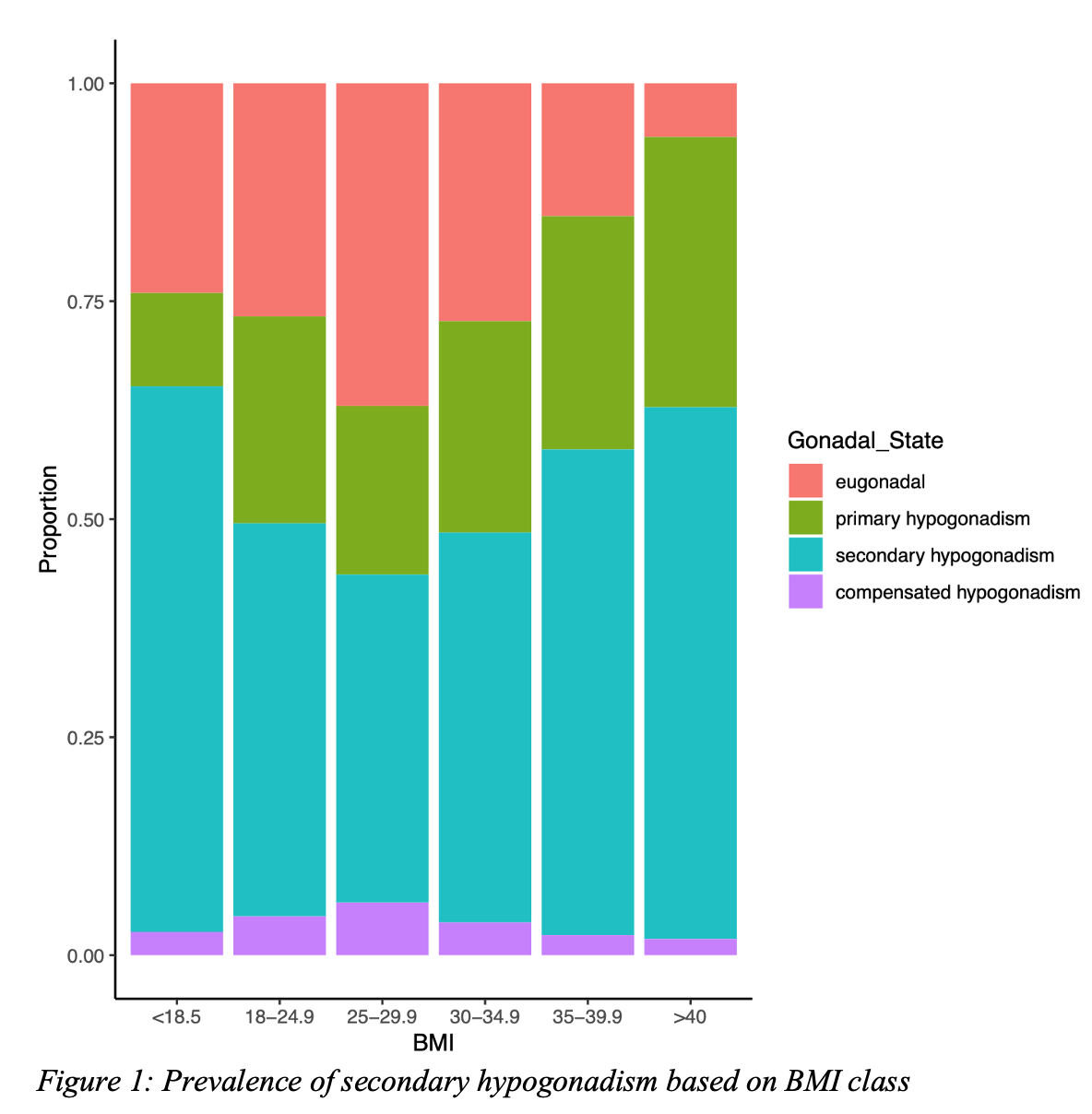
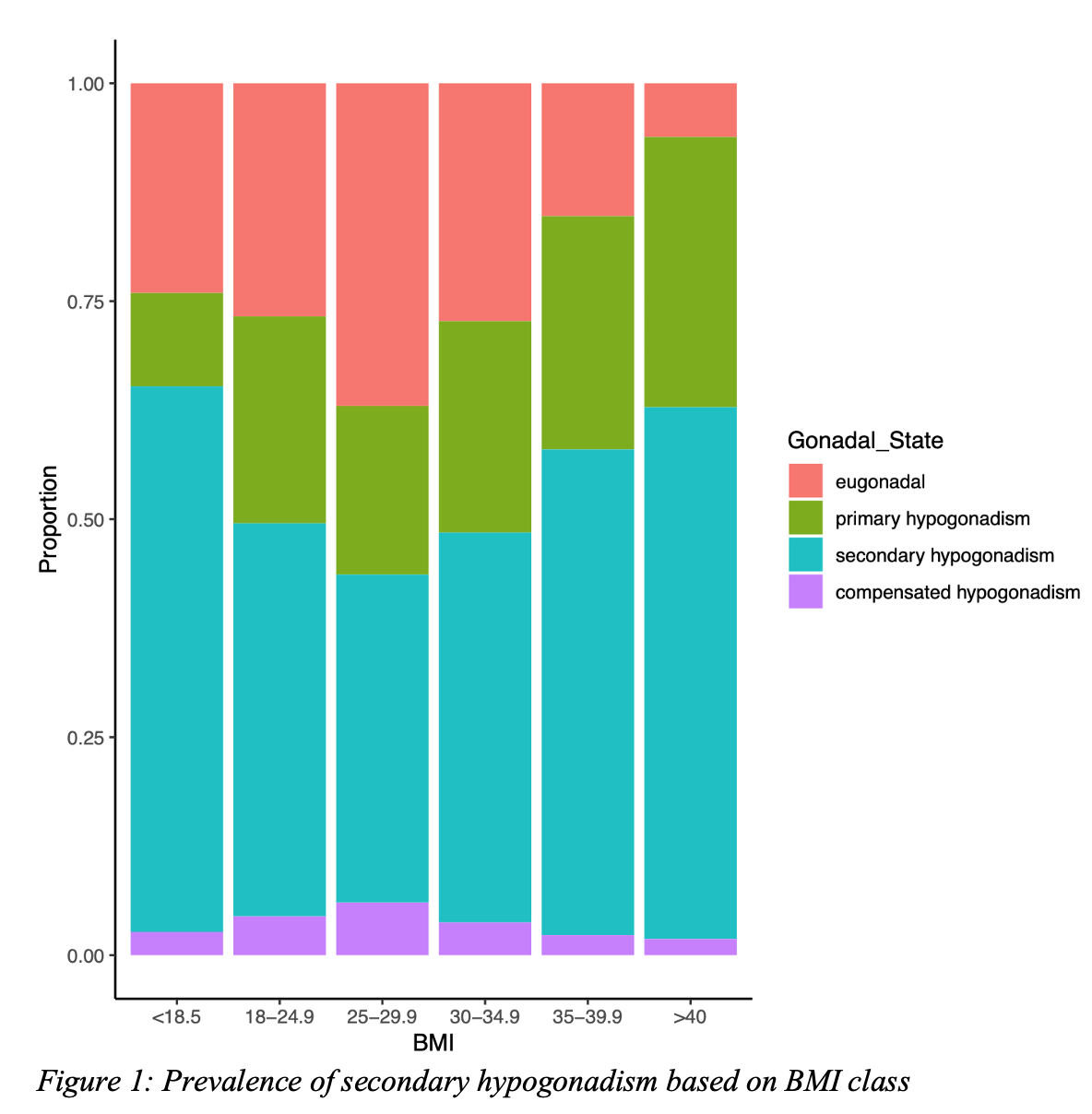
Results: Among 7,211 men studied, 45.7%, 22.6%, and 4.4% were classified as secondary, primary, and compensated hypogonadism, respectively. We found that 56% and 61% of men in obesity class II and III, respectively, and 63% underweight men had secondary hypogonadism (Fig 1). The Pearson’s Chi-Squared test had a X2 = 374.1 (p < .001, df = 15).
Conclusions: Males at BMI extremes (i.e., Obesity Class II-III and underweight) have a higher prevalence of secondary hypogonadism. Obese men may have secondary hypogonadism due to decreased levels of circulating estradiol and sex hormone binding globulin, and leptin resistance in the hypothalamus. For underweight men, this process may represent an adaptive response to an energy deficit, involving suppression of the hypothalamus due to dysregulation of ghrelin, leptin, and pro-inflammatory cytokines. These findings support screening for secondary hypogonadism in obese men to recommend weight loss and TRT to reduce cardiovascular related mortality, while increasing caloric intake in underweight men to improve libido and sexual function.
Source of Funding: This work was supported by the National Institutes of Health Grant R01 DK130991 and Clinician Scientist Development Grant from the American Cancer Society to Ranjith Ramasamy.
Methods: We constructed a retrospective database with men who had their BMI, morning T and LH levels measured during a visit to a urology clinic at a tertiary academic medical center between 2011-2020. Men previously on testosterone replacement therapy (TRT), Clomiphene, or Anastrozole were excluded. Chi-squared analysis was conducted in R (4.1.1).
Results: Among 7,211 men studied, 45.7%, 22.6%, and 4.4% were classified as secondary, primary, and compensated hypogonadism, respectively. We found that 56% and 61% of men in obesity class II and III, respectively, and 63% underweight men had secondary hypogonadism (Fig 1). The Pearson’s Chi-Squared test had a X2 = 374.1 (p < .001, df = 15).
Conclusions: Males at BMI extremes (i.e., Obesity Class II-III and underweight) have a higher prevalence of secondary hypogonadism. Obese men may have secondary hypogonadism due to decreased levels of circulating estradiol and sex hormone binding globulin, and leptin resistance in the hypothalamus. For underweight men, this process may represent an adaptive response to an energy deficit, involving suppression of the hypothalamus due to dysregulation of ghrelin, leptin, and pro-inflammatory cytokines. These findings support screening for secondary hypogonadism in obese men to recommend weight loss and TRT to reduce cardiovascular related mortality, while increasing caloric intake in underweight men to improve libido and sexual function.
Source of Funding: This work was supported by the National Institutes of Health Grant R01 DK130991 and Clinician Scientist Development Grant from the American Cancer Society to Ranjith Ramasamy.

.jpg)
.jpg)