Back
Poster, Podium & Video Sessions
Moderated Poster
MP22: Trauma/Reconstruction/Diversion: Urethral Reconstruction (including Stricture, Diverticulum) I
MP22-06: The Impact of Prostate Cancer Disease Progression and Salvage or Adjuvant Treatment on Artificial Urinary Sphincter Device Outcomes
Saturday, May 14, 2022
8:45 AM – 10:00 AM
Location: Room 228
Shree Agrawal*, Hanson Zhao, Joao Pedro Emrich Accioly, Hadley Wood, Kenneth Angermeier, Cleveland, OH
Poster Presenter(s)
Introduction: While utilization of artificial urinary sphincter (AUS) for post prostate cancer intervention incontinence can improve quality of life, AUS placement in men with prostate cancer (CaP) progression to biochemical recurrence (BR) or distant metastatic disease (DM) with respect to AUS outcomes has yet to be characterized.
Methods: Retrospective review of patients who underwent AUS implantation from 1/2009-8/2021 was performed. Demographics, comorbidities, CaP treatment, pathology, progression, timing of AUS following primary intervention, surgical characteristics, incontinence outcomes and device revisions were assessed by chi-square and Pearson’s t-test analyses. Multivariable Cox proportional hazards and Kaplan Meier models were used to assess time to AUS device revision by CaP progression.
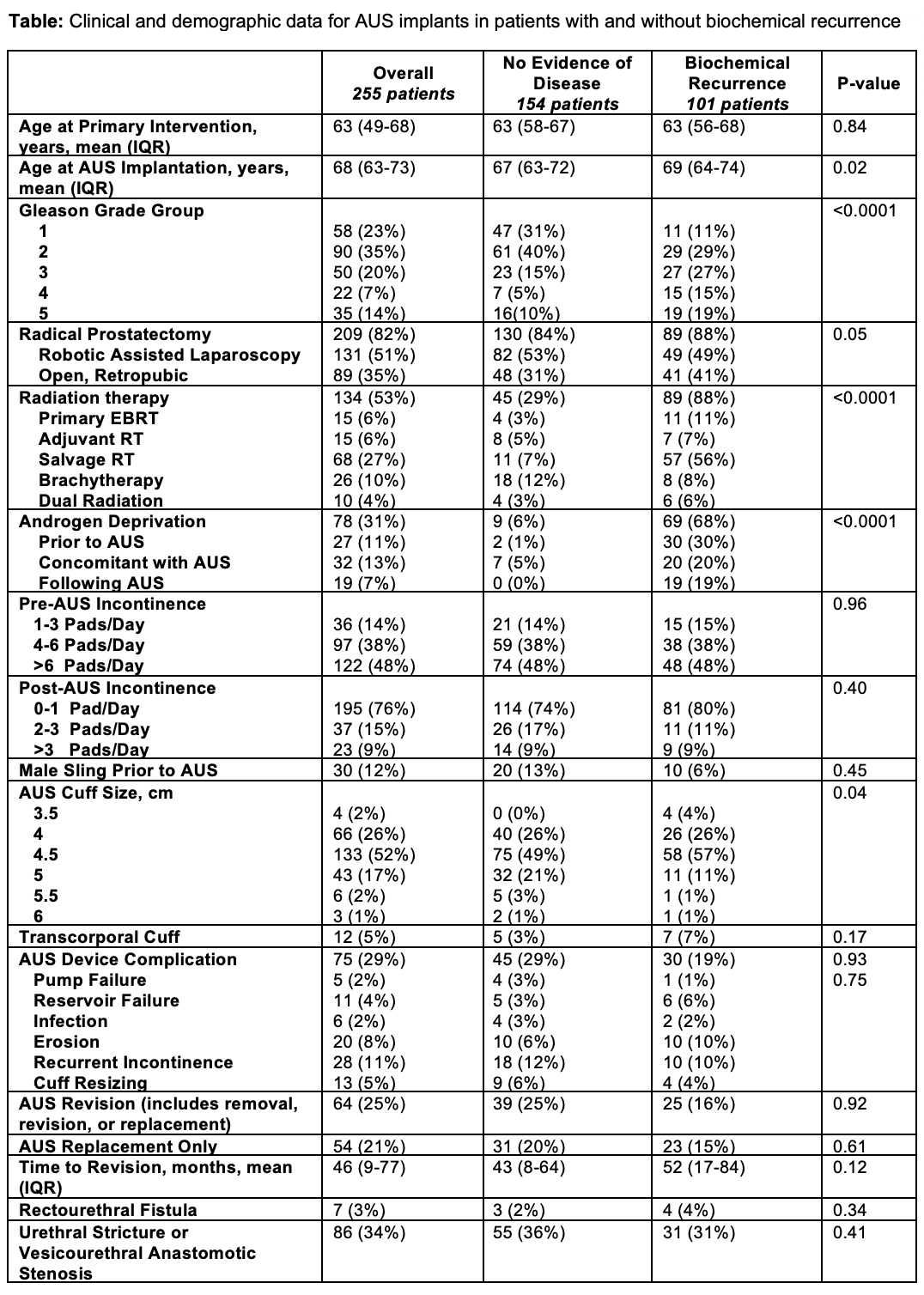
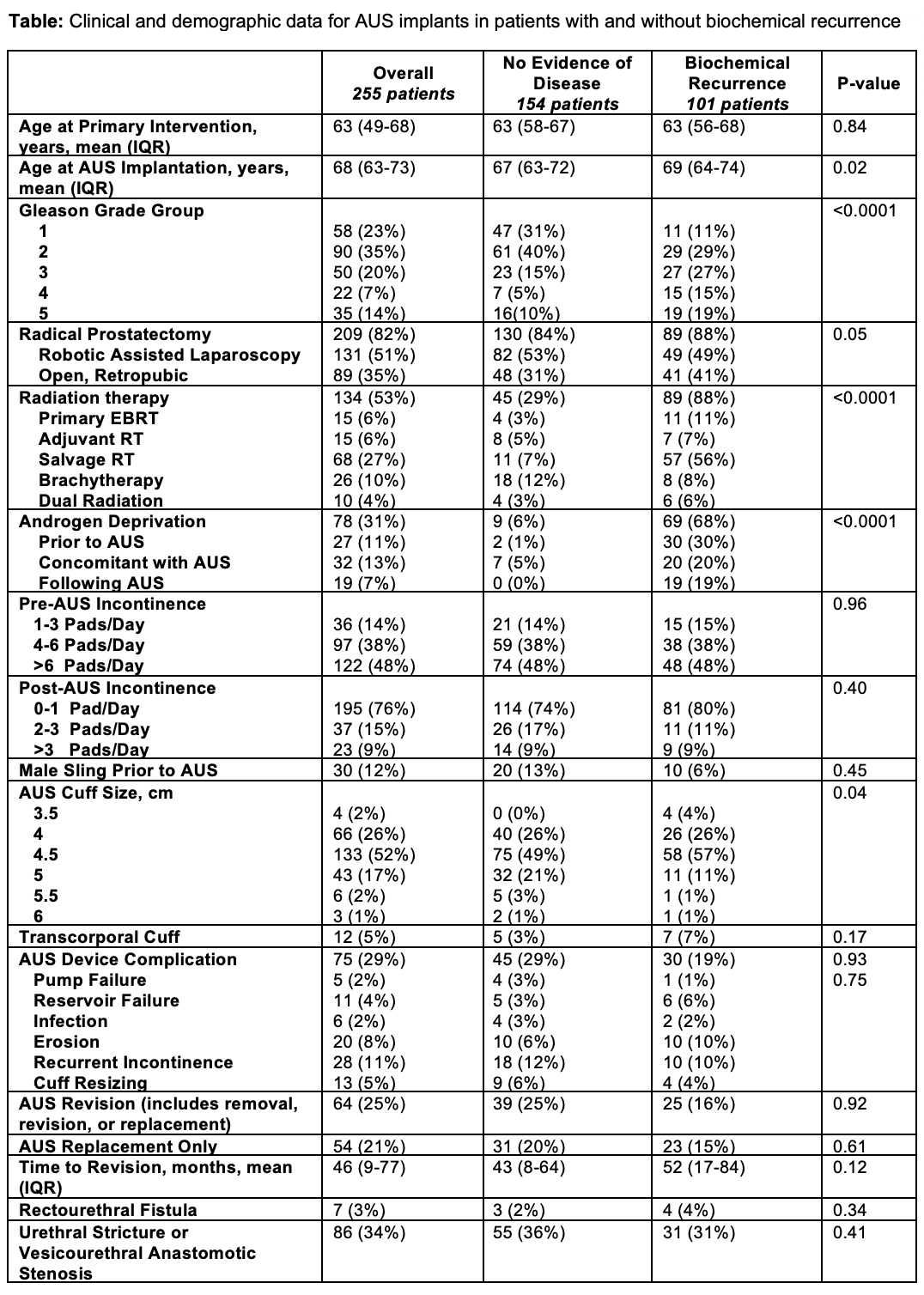
Results: We identified 526 patients who underwent AUS implantation, 255 had complete CaP and AUS characteristics as summarized in the table. Mean follow up from AUS and primary CaP treatment was 56 and 118 months, respectively. Among 134 patients treated with radiation, 40 developed AUS complications with 11 erosions and 11 with recurrent incontinence (p = 0.21). In 78 patients treated with androgen deprivation therapy (ADT), AUS complications were noted in 22 with 7 erosions and 6 with recurrent incontinence, prompting revision (p = 0.77). BR occurred in 101 patients (40%), with 16% requiring AUS revision (p = 0.92). DM developed in 28 patients (11%), with 8 undergoing AUS after DM diagnosis. On univariate analysis, only transcorporal cuff use [HR 3.6 (95% CI 1.7-7.3), p = 0.001] significantly correlated with AUS revision.
There was no significant difference in continence rates following AUS for patients who underwent prostatectomy, radiation therapy, ADT, or who developed BR or DM. A majority (76%) reported 0-1 pads/day at last follow up. AUS durability for those with BR, by 2 years was 92%, 5 years 85%, and by 10 years 60% (p = 0.55). In DM, this was 96% by 2 years, 90% by 5 years, and 71% by 10 years (p = 0.26).
Conclusions: There were no significant differences in AUS outcomes between patients without CaP disease progression and those with BR, local recurrence, or DM. Based on this data, AUS implantation in patients undergoing salvage or adjuvant therapy may still be an effective procedure.
Source of Funding: None
Methods: Retrospective review of patients who underwent AUS implantation from 1/2009-8/2021 was performed. Demographics, comorbidities, CaP treatment, pathology, progression, timing of AUS following primary intervention, surgical characteristics, incontinence outcomes and device revisions were assessed by chi-square and Pearson’s t-test analyses. Multivariable Cox proportional hazards and Kaplan Meier models were used to assess time to AUS device revision by CaP progression.
Results: We identified 526 patients who underwent AUS implantation, 255 had complete CaP and AUS characteristics as summarized in the table. Mean follow up from AUS and primary CaP treatment was 56 and 118 months, respectively. Among 134 patients treated with radiation, 40 developed AUS complications with 11 erosions and 11 with recurrent incontinence (p = 0.21). In 78 patients treated with androgen deprivation therapy (ADT), AUS complications were noted in 22 with 7 erosions and 6 with recurrent incontinence, prompting revision (p = 0.77). BR occurred in 101 patients (40%), with 16% requiring AUS revision (p = 0.92). DM developed in 28 patients (11%), with 8 undergoing AUS after DM diagnosis. On univariate analysis, only transcorporal cuff use [HR 3.6 (95% CI 1.7-7.3), p = 0.001] significantly correlated with AUS revision.
There was no significant difference in continence rates following AUS for patients who underwent prostatectomy, radiation therapy, ADT, or who developed BR or DM. A majority (76%) reported 0-1 pads/day at last follow up. AUS durability for those with BR, by 2 years was 92%, 5 years 85%, and by 10 years 60% (p = 0.55). In DM, this was 96% by 2 years, 90% by 5 years, and 71% by 10 years (p = 0.26).
Conclusions: There were no significant differences in AUS outcomes between patients without CaP disease progression and those with BR, local recurrence, or DM. Based on this data, AUS implantation in patients undergoing salvage or adjuvant therapy may still be an effective procedure.
Source of Funding: None

.jpg)
.jpg)
