Back
Poster, Podium & Video Sessions
Moderated Poster
MP22: Trauma/Reconstruction/Diversion: Urethral Reconstruction (including Stricture, Diverticulum) I
MP22-09: Urethral Stricture/Stenosis as a Complication of High Intensity Focused Ultrasound of the Prostate: What is the Overall Patient Experience?
Saturday, May 14, 2022
8:45 AM – 10:00 AM
Location: Room 228
David Barham*, Orange, CA, John Barnard, Morgantown, WV, Joel Gelman, Orange, CA

David W. Barham, MD
University of California, Irvine
Poster Presenter(s)
Introduction: High Intensity Focused Ultrasound (HIFU) is an emerging treatment option for localized prostate cancer. Urethral stricture/stenosis develops in about 19% of patients on average, and is generally treated endoscopically. The literature does not describe in any detail the location of obstruction, treatment success rate, or impact on the patient's quality of life(QOL). Our objective was to analyze patients with HIFU stricture/stenosis to characterize location, management, and patient reported satisfaction.
Methods: Patients with a history of HIFU requesting consultation for stricture were identified from 2010-2020. Demographic and prior treatment data were recorded. Patients who presented for evaluation underwent cystoscopy, retrograde urethrogram, and voiding cystourethrogram. Patients, including those who did not present for in-person consultation, were followed longitudinally to assess long-term outcomes and QOL.
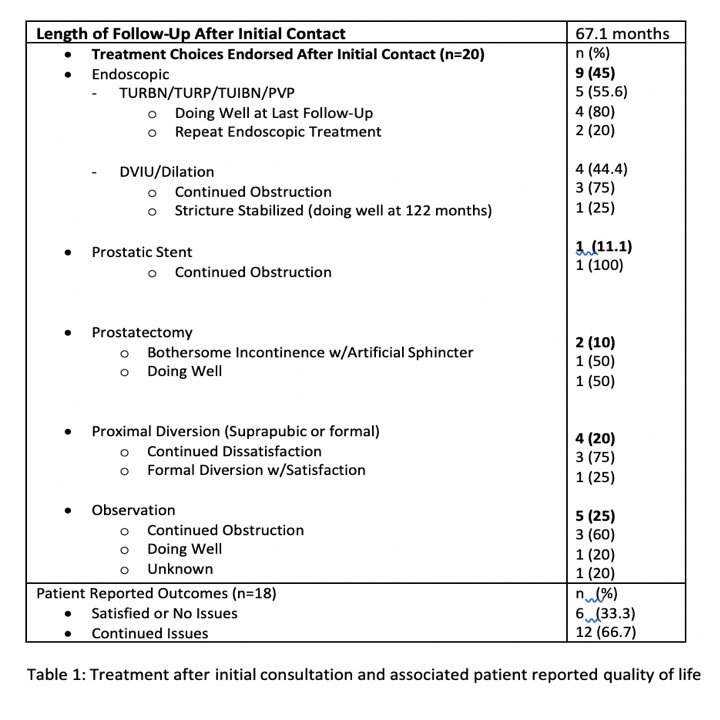
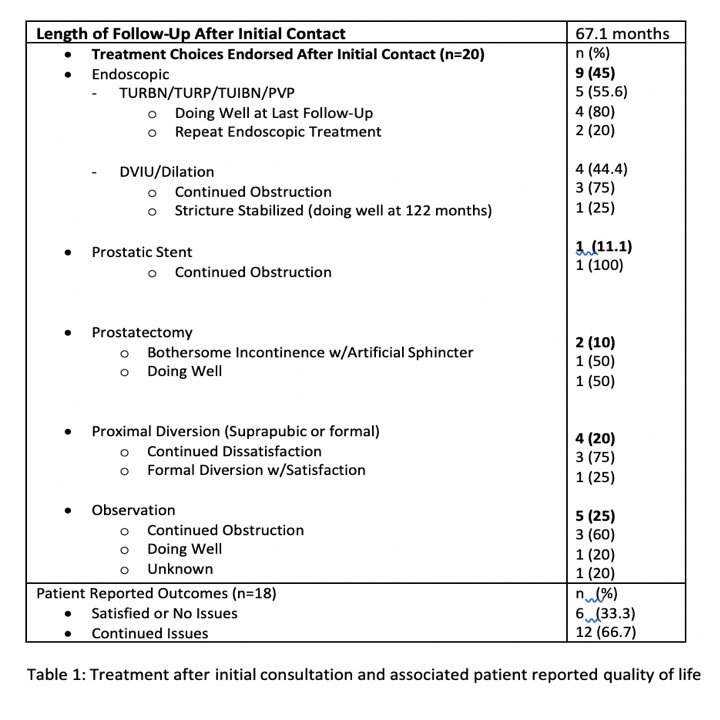
Results: 29 patients were identified with a mean age of 65.8 years. Prior to initial consultation, a total of 86.2% of patients had at least one failed surgical intervention at a mean of 45.1 months post-HIFU. Seventeen patients underwent urethral evaluation and 94.1% had strictures that included but were not necessarily limited to the prostatic urethra. Additionally, 35.3% had bladder neck stenosis, 23.5% had membranous stenosis, and 17.6% had anterior urethral strictures. 20 patients underwent various treatments post-evaluation, favoring endoscopic therapy (45%) and proximal diversion (20%) at a mean of 67.1 months follow-up (Table 1). Only 33.3% reported satisfaction with urinary symptoms.
Conclusions: Urethral narrowing post-HIFU appears to overwhelmingly involve the prostatic urethra. Patients usually have a significant treatment burden over a prolonged period and are often managed with repeated endoscopic or extirpative prostatic surgery. Some undergo urinary diversion, but most patients with HIFU strictures experience a diminished QOL due to persistent urinary symptoms.
Source of Funding: None
Methods: Patients with a history of HIFU requesting consultation for stricture were identified from 2010-2020. Demographic and prior treatment data were recorded. Patients who presented for evaluation underwent cystoscopy, retrograde urethrogram, and voiding cystourethrogram. Patients, including those who did not present for in-person consultation, were followed longitudinally to assess long-term outcomes and QOL.
Results: 29 patients were identified with a mean age of 65.8 years. Prior to initial consultation, a total of 86.2% of patients had at least one failed surgical intervention at a mean of 45.1 months post-HIFU. Seventeen patients underwent urethral evaluation and 94.1% had strictures that included but were not necessarily limited to the prostatic urethra. Additionally, 35.3% had bladder neck stenosis, 23.5% had membranous stenosis, and 17.6% had anterior urethral strictures. 20 patients underwent various treatments post-evaluation, favoring endoscopic therapy (45%) and proximal diversion (20%) at a mean of 67.1 months follow-up (Table 1). Only 33.3% reported satisfaction with urinary symptoms.
Conclusions: Urethral narrowing post-HIFU appears to overwhelmingly involve the prostatic urethra. Patients usually have a significant treatment burden over a prolonged period and are often managed with repeated endoscopic or extirpative prostatic surgery. Some undergo urinary diversion, but most patients with HIFU strictures experience a diminished QOL due to persistent urinary symptoms.
Source of Funding: None

.jpg)
.jpg)