Back
Poster, Podium & Video Sessions
Moderated Poster
MP22: Trauma/Reconstruction/Diversion: Urethral Reconstruction (including Stricture, Diverticulum) I
MP22-18: Revision Urethroplasty after failed excision and primary anastomosis and tissue transfer repair for bulbar urethral strictures: Outcome Analysis
Saturday, May 14, 2022
8:45 AM – 10:00 AM
Location: Room 228
David Barham*, Orange, CA, Aron Liaw, Detroit, MI, Joel Gelman, Orange, CA

David W. Barham, MD
University of California, Irvine
Poster Presenter(s)
Introduction: The published short and long-term success rates for anastomotic and dorsal buccal onlay urethroplasty for the treatment of bulbar strictures are as high as 95-99% at centers of excellence. As urethroplasty is being performed with increased frequency, more patients are presenting for re-do urethroplasty with highly complex and/or long strictures, especially after surgery performed by urologists without fellowship training and/or specialization in Male Reconstructive Urology. We report our 20-year experience and long-term outcomes with revision surgery when patients present to our institution after failed excision and primary anastomosis (EPA) or tissue transfer bulbar urethroplasty.
Methods: We reviewed our IRB approved, prospectively maintained database for patients who had repeat urethroplasty for bulbar or distal membranous stricture. Success was defined as a urethra >16Fr on followup cystoscopy and absence of obstructive voiding symptoms.
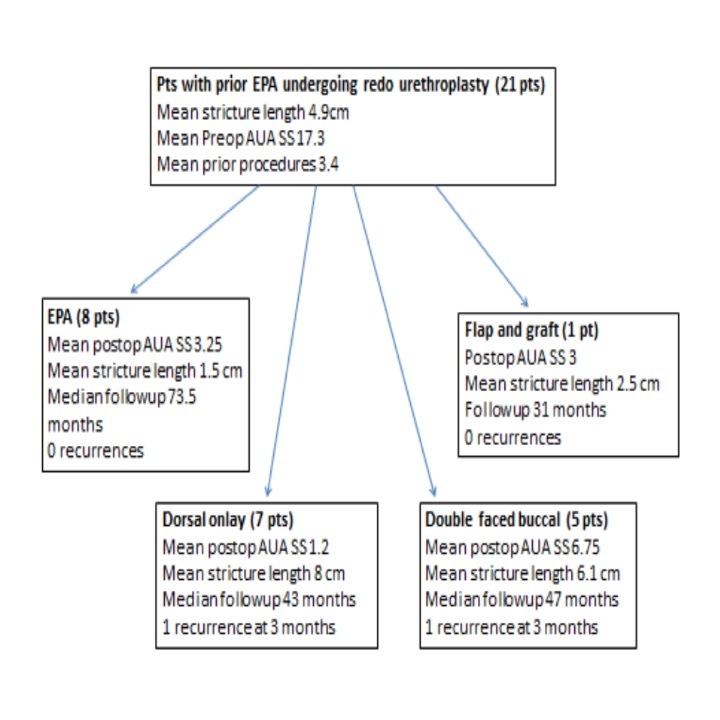
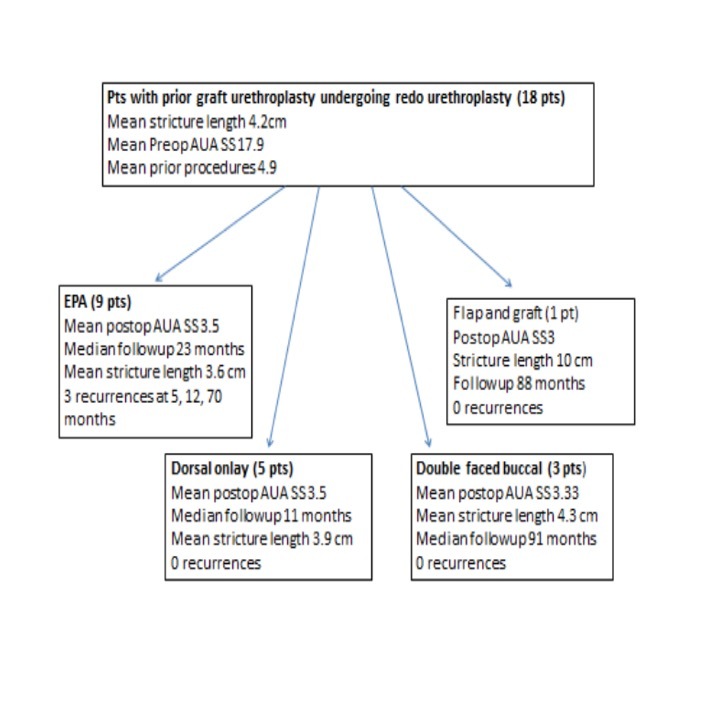
Results: 43 patients were identified, with a mean followup of 66 months (4-210). 21/43 (48%) had previously undergone EPA. Of these, 13/21 (62%) had a mean stricture length 6.8 cm, and underwent buccal graft urethroplasty as a revision. Conversely, 18/43 (42%) had previously undergone a graft urethroplasty, and of those, 9/18 (50%) underwent EPA as a salvage operation. The remaining 4 patients had prior flap surgery (2/43), or multiple different prior urethroplasties (2/43). 6/43 (14%) had documented recurrence of stricture, 3/6 of which were in the group that had previous graft urethroplasty and had EPA as a revision.
Conclusions: Most patients with failed anastomotic urethroplasty had long stricture length and required tissue transfer for revision, indicating increased complexity after failure. Patients with failed graft urethroplasty did well when their revision was done with tissue transfer, but there was a higher failure rate in those who underwent anastomotic repair after a failed graft.
Source of Funding: None
Methods: We reviewed our IRB approved, prospectively maintained database for patients who had repeat urethroplasty for bulbar or distal membranous stricture. Success was defined as a urethra >16Fr on followup cystoscopy and absence of obstructive voiding symptoms.
Results: 43 patients were identified, with a mean followup of 66 months (4-210). 21/43 (48%) had previously undergone EPA. Of these, 13/21 (62%) had a mean stricture length 6.8 cm, and underwent buccal graft urethroplasty as a revision. Conversely, 18/43 (42%) had previously undergone a graft urethroplasty, and of those, 9/18 (50%) underwent EPA as a salvage operation. The remaining 4 patients had prior flap surgery (2/43), or multiple different prior urethroplasties (2/43). 6/43 (14%) had documented recurrence of stricture, 3/6 of which were in the group that had previous graft urethroplasty and had EPA as a revision.
Conclusions: Most patients with failed anastomotic urethroplasty had long stricture length and required tissue transfer for revision, indicating increased complexity after failure. Patients with failed graft urethroplasty did well when their revision was done with tissue transfer, but there was a higher failure rate in those who underwent anastomotic repair after a failed graft.
Source of Funding: None

.jpg)
.jpg)