Back
Poster, Podium & Video Sessions
Moderated Poster
MP23: Bladder Cancer: Invasive III
MP23-09: Acute kidney injury and its duration in patients treated with radical cystectomy in the Enhanced Recovery After Surgery Era: Optimizing the selection of patients for restrictive fluid therapy
Saturday, May 14, 2022
8:45 AM – 10:00 AM
Location: Room 225
Alberto Martini, Riccardo Leni*, Francesco Pellegrino, Giuseppe Basile, Simone Scuderi, Mario De Angelis, Luigi Nocera, Giuseppe Rosiello, Giorgio Gandaglia, Milan, Italy, Andrea Gallina, Lugano, Switzerland, Francesco Montorsi, Alberto Briganti, Marco Moschini, Milan, Italy

Riccardo Leni, MD
IRCCS Ospedale San Raffaele
Poster Presenter(s)
Introduction: Acute kidney injury (AKI) is not an uncommon occurrence after Radical cystectomy (RC). An integral part of the enhanced recovery after surgery (ERAS) protocol is restrictive fluid therapy in the postoperative period. Yet, this might enhance the occurrence of postoperative AKI and not all patients might benefit from it. We aimed to investigate whether AKI and its duration is associated with worse renal functional outcomes to identify individuals that should not be treated with restrictive fluid therapy following RC.
Methods: Patients who underwent RC at a single high-volume institution between 2015-2020 whose postoperative course followed the ERAS protocol were evaluated. The LOWESS and Cox regression were used to assess the impact of AKI (according to the RIFLE criteria: i.e., more than 25% reduction in preoperative baseline eGFR or more than 1.5-fold increase in preoperative creatinine) and its duration (0-3 vs more than 3 days) on significant renal impairment (eGFR reduction of greater or equal to 25%) at 12 months. Finally, we evaluated predictors of AKI duration =4 days as this was associated with worse outcomes in terms of renal function
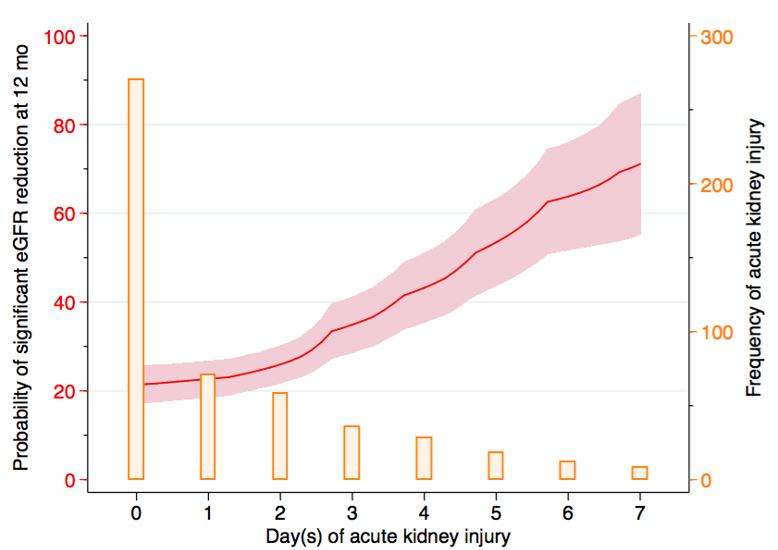
Results: Among 501 patients, 46% developed postoperative AKI. Patients who developed AKI were older (71 vs 69 years-old, p=0.024), and had higher Charlson Comorbidity Index (CCI>2 in 54 vs 38%, p=0.002) . Baseline eGFR, type of surgical approach (open vs robot), use of neoadjuvant treatment were balanced between groups (all p>0.05). Overall, 24% had a significant decline in renal function at 12-month. Figure 1 displays the correlation between the probability of eGFR reduction at 12-month with the duration of AKI and the relative frequency of AKI across the postoperative days. A prolonged duration of postoperative AKI (= 4 days) was predictor of 12-month decline (HR 7.25, 95%CI 3.93,13.4, p<0.001). A high comorbidity burden (CCI=3) was associated with prolonged postoperative AKI (OR 1.71, 95%CI 1.16,2.95, p=0.04).
Conclusions: Prolonged AKI (=4 days) is associated with worse renal functional outcome after RC. The sole predictor of prolonged AKI was CCI=3. Patients with a high comorbidity burden should not be treated with restrictive fluid therapy as part of the ERAS protocol following RC.
Source of Funding: no
Methods: Patients who underwent RC at a single high-volume institution between 2015-2020 whose postoperative course followed the ERAS protocol were evaluated. The LOWESS and Cox regression were used to assess the impact of AKI (according to the RIFLE criteria: i.e., more than 25% reduction in preoperative baseline eGFR or more than 1.5-fold increase in preoperative creatinine) and its duration (0-3 vs more than 3 days) on significant renal impairment (eGFR reduction of greater or equal to 25%) at 12 months. Finally, we evaluated predictors of AKI duration =4 days as this was associated with worse outcomes in terms of renal function
Results: Among 501 patients, 46% developed postoperative AKI. Patients who developed AKI were older (71 vs 69 years-old, p=0.024), and had higher Charlson Comorbidity Index (CCI>2 in 54 vs 38%, p=0.002) . Baseline eGFR, type of surgical approach (open vs robot), use of neoadjuvant treatment were balanced between groups (all p>0.05). Overall, 24% had a significant decline in renal function at 12-month. Figure 1 displays the correlation between the probability of eGFR reduction at 12-month with the duration of AKI and the relative frequency of AKI across the postoperative days. A prolonged duration of postoperative AKI (= 4 days) was predictor of 12-month decline (HR 7.25, 95%CI 3.93,13.4, p<0.001). A high comorbidity burden (CCI=3) was associated with prolonged postoperative AKI (OR 1.71, 95%CI 1.16,2.95, p=0.04).
Conclusions: Prolonged AKI (=4 days) is associated with worse renal functional outcome after RC. The sole predictor of prolonged AKI was CCI=3. Patients with a high comorbidity burden should not be treated with restrictive fluid therapy as part of the ERAS protocol following RC.
Source of Funding: no

.jpg)
.jpg)