Back
Poster, Podium & Video Sessions
Moderated Poster
MP23: Bladder Cancer: Invasive III
MP23-10: Longitudinal assessment of 1-yr Health Related Quality of Life outcomes: head to head comparison between Open and Robot-Assisted Radical Cystectomy with totally intracorporeal Urinary Diversion from a single center randomised controlled trial
Saturday, May 14, 2022
8:45 AM – 10:00 AM
Location: Room 225
Riccardo Mastroianni*, Gabriele Tuderti, Umberto Anceschi, Alfredo Maria Bove, Aldo Brassetti, Mariaconsiglia Ferriero, Leonardo Misuraca, Salvatore Guaglianone, Michele Gallucci, Giuseppe Simone, Rome, Italy

Riccardo Mastroianni, MD
IRCCS "Regina Elena" National Cancer Institute
Poster Presenter(s)
Introduction: Radical Cystectomy (RC) with urinary diversion (UD) is still considered a complex surgery associated with significant morbidity and impact on HRQoL. In this study, we performed analysis of 1yr HRQoL outcomes from an ongoing RCT comparing ORC and RARC with totally intracorporeal UD (NCT03434132).
Methods: Patients were eligible for randomization if they had a diagnostic TURBt cT2-4cN0cM0, or recurrent HG NMIBC and no anesthesiologic contraindications to robotic surgery. Between Jan 2018 and Sept 2020, patients were enrolled with a covariate adaptive randomization process based on: BMI, ASA, preoperative Hgb, UD (padua ileal bladder or conduit), neoadjuvant chemo and cTstage. Data from questionnaires EORTCgeneric QLQ-C30; QLQ-BLM30 were collected. Normally distributed HRQoL continuous variables were compared with paired t test. A generalized linear mixed effect regression (GLMER) model including a random effect at patients’ level was implemented to test variation of HRQoL items along time and between the two surgical approaches.
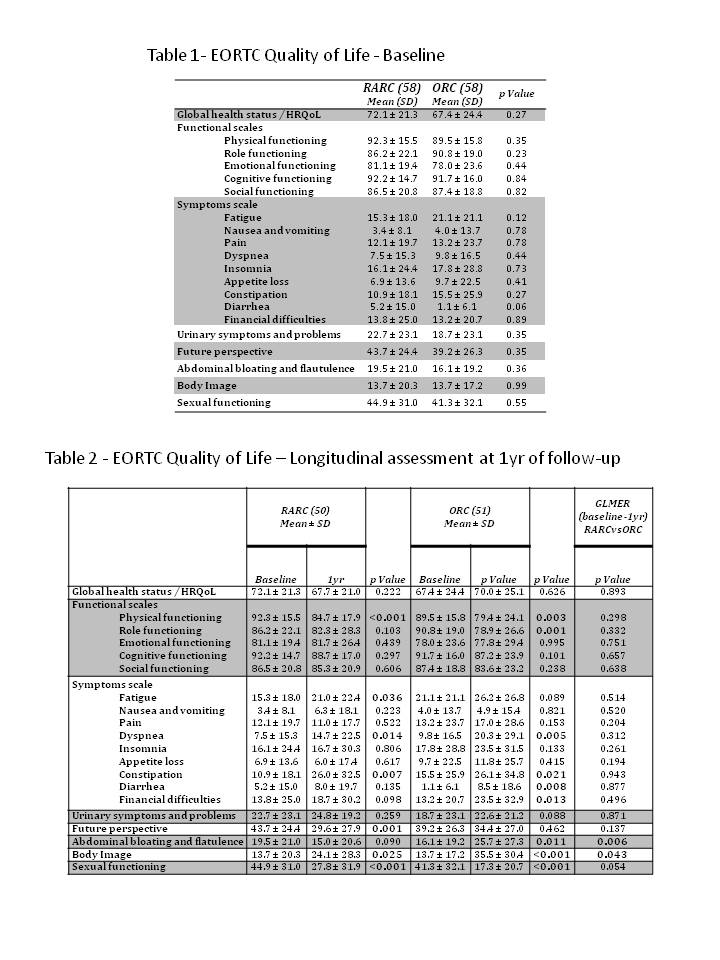
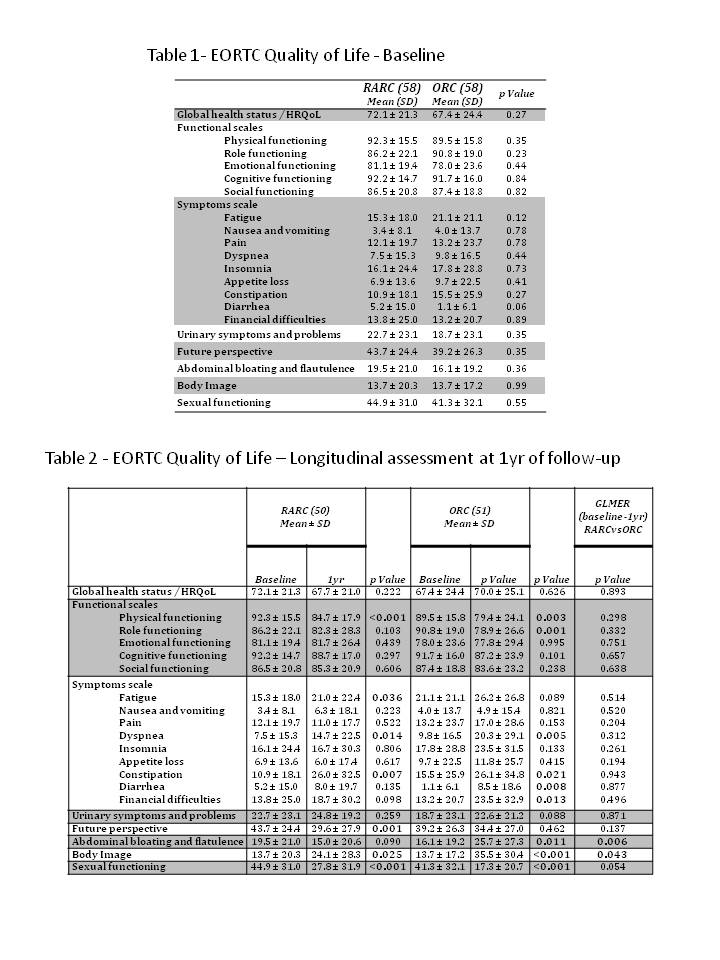
Results: Out of 116 patients enrolled, 101 with a 1yr minimum follow-up length were included. 13 patients died within 1yr after surgery (RARC: 7 vs ORC: 6), 2 patients were lost to follow-up. Baseline HRQoL outcomes were reported (Tab.1). At 1yr HRQoL evaluation, both cohorts reported significant worsening in terms of physical, and sexual functioning, and a significant impairment of dyspnea, constipation and body image (all p<0.05, Tab. 2). Patients receiving ORC were more likely to report 1yr impairment of role functioning, diarrhea, financial difficulties, and abdominal bloating and flatulence (all p<0.013). Otherwise, patients receiving RARC reported a significant 1yr impairment in terms of fatigue and a significant improvement in future perspectives (all p<0.036). At GLMER analysis, ORC cohort displayed a significant impairment in terms of abdominal bloating and flatulence and body image (p < 0.043) compared with RARC arm.
Conclusions: At 1yr HRQoL analysis, patients who underwent RARC-iUD reported significant benefits in terms of body image and abdominal bloating and flatulence compared to patients who underwent ORC.
Source of Funding: no
Methods: Patients were eligible for randomization if they had a diagnostic TURBt cT2-4cN0cM0, or recurrent HG NMIBC and no anesthesiologic contraindications to robotic surgery. Between Jan 2018 and Sept 2020, patients were enrolled with a covariate adaptive randomization process based on: BMI, ASA, preoperative Hgb, UD (padua ileal bladder or conduit), neoadjuvant chemo and cTstage. Data from questionnaires EORTCgeneric QLQ-C30; QLQ-BLM30 were collected. Normally distributed HRQoL continuous variables were compared with paired t test. A generalized linear mixed effect regression (GLMER) model including a random effect at patients’ level was implemented to test variation of HRQoL items along time and between the two surgical approaches.
Results: Out of 116 patients enrolled, 101 with a 1yr minimum follow-up length were included. 13 patients died within 1yr after surgery (RARC: 7 vs ORC: 6), 2 patients were lost to follow-up. Baseline HRQoL outcomes were reported (Tab.1). At 1yr HRQoL evaluation, both cohorts reported significant worsening in terms of physical, and sexual functioning, and a significant impairment of dyspnea, constipation and body image (all p<0.05, Tab. 2). Patients receiving ORC were more likely to report 1yr impairment of role functioning, diarrhea, financial difficulties, and abdominal bloating and flatulence (all p<0.013). Otherwise, patients receiving RARC reported a significant 1yr impairment in terms of fatigue and a significant improvement in future perspectives (all p<0.036). At GLMER analysis, ORC cohort displayed a significant impairment in terms of abdominal bloating and flatulence and body image (p < 0.043) compared with RARC arm.
Conclusions: At 1yr HRQoL analysis, patients who underwent RARC-iUD reported significant benefits in terms of body image and abdominal bloating and flatulence compared to patients who underwent ORC.
Source of Funding: no

.jpg)
.jpg)