Back
Poster, Podium & Video Sessions
Moderated Poster
MP23: Bladder Cancer: Invasive III
MP23-11: Perioperative Complications after Radical Cystectomy for Bladder Cancer: an International Multicenter Collaboration
Saturday, May 14, 2022
8:45 AM – 10:00 AM
Location: Room 225
Chiara Lonati*, Brescia, Italy, Luca Afferi, Lucerne, Switzerland, Ettore Di Trapani, Milan, Italy, Stefania Zamboni, Claudio Simeone, Brescia, Italy, Alberto Briganti, Francesco Montorsi, Milan, Italy, Giuseppe Simone, Rome, Italy, Francesco Soria, Turin, Italy, M. Carmen Mir, Valencia, Spain, Rafael Sanchez-Salas, Paris, France, Mathieu Roumiguié, Toulouse, France, Alessandro Antonelli, Verona, Italy, Kees Hendricksen, Amsterdam, Netherlands, Agostino Mattei, Christian D. Fankhauser, Roberto Carando, Lucerne, Switzerland, Jeremy Y.C. Teoh, Hong Kong, China, People's Republic of, Shahrokh F. Shariat, Vienna, Austria, Simone Albisinni, Bruxelles, Belgium, Rodolfo Hurle, Milan, Italy, Angelo Peroni, Brescia, Italy, Evanguelos Xylinas, Paris, France, Wojciech Krajewski, Wroclaw, Poland, Morgan Roupret, Paris, France, Marco Moschini, Milan, Italy

Chiara Lonati, MD
Spedali Civili of Brescia
Poster Presenter(s)
Introduction: To evaluate incidence of perioperative complications after radical cystectomy (RC) for bladder cancer (BCa), assessing risk factors for intra- and post-operative complications
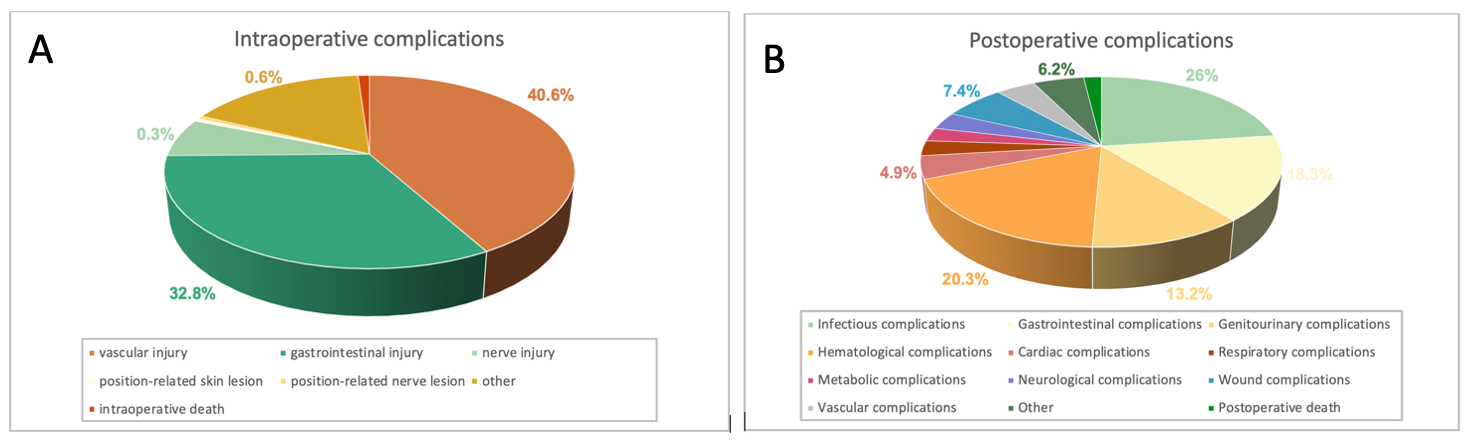
Methods: We retrospectively analyzed data of 4,731 patients treated with RC for BCa among 25 tertiary referral centers between 2001 and 2020. Intra-operative complications included gastrointestinal (GI), vascular, nerve injury, position-related skin and peripheral nerve lesion, and death. Post-operative complications were coded as early ( <30 days) and late (30-90 days) complications, including infectious, GI, genitourinary (GU), hematological, cardiac, wound complications, and death. Multivariable logistic regression models (LGRs) were applied to evaluate independent predictors of intra- and post-operative complications; covariates consisted of demographic features and perioperative outcomes
Results: Open, laparoscopic, and robotic RC were performed in 69.1%, 10.7%, 20.2% of patients, respectively; conversion from robotic to open technique was recorded in 3 patients. Overall, 3.8% of patients experienced intra-operative complications: vascular injury occurred in 40.6% of cases, followed by GI injury (32.8%); intra-operative death occurred in 1.1% of cases (Fig. 1A). Overall, 64.1% of patients experienced post-operative complications (early: 57.6% and late: 17.9%). Infectious complications occurred in 26% of patients, followed by anemia (20.3%), and GI (18.3%) complications. Death due to early and late complications occurred in 1.5% and 0.6% of patients, respectively (Fig. 1B). At multivariable LGMs prior abdominal surgery (odd ratio [OR]: 1.87; p=0.005) and surgeon experience (>250 RC/surgeon: OR: 0.27; p=0.003) were independent predictors of intra-operative complications, while female gender (OR: 0.66; p=0.03), anticoagulant therapy (OR: 2.05; p=0.04), and post-operative transfusions (OR: 4.84; p<0.001) were independent predictors of post-operative complications. Surgical RC technique was not an independent predictor of complication
Conclusions: RC is still burden with an increased rate of perioperative complications. Risk factors for perioperative complications include scarce surgeon experience, prior abdominal surgery, and post-operative transfusions
Source of Funding: None
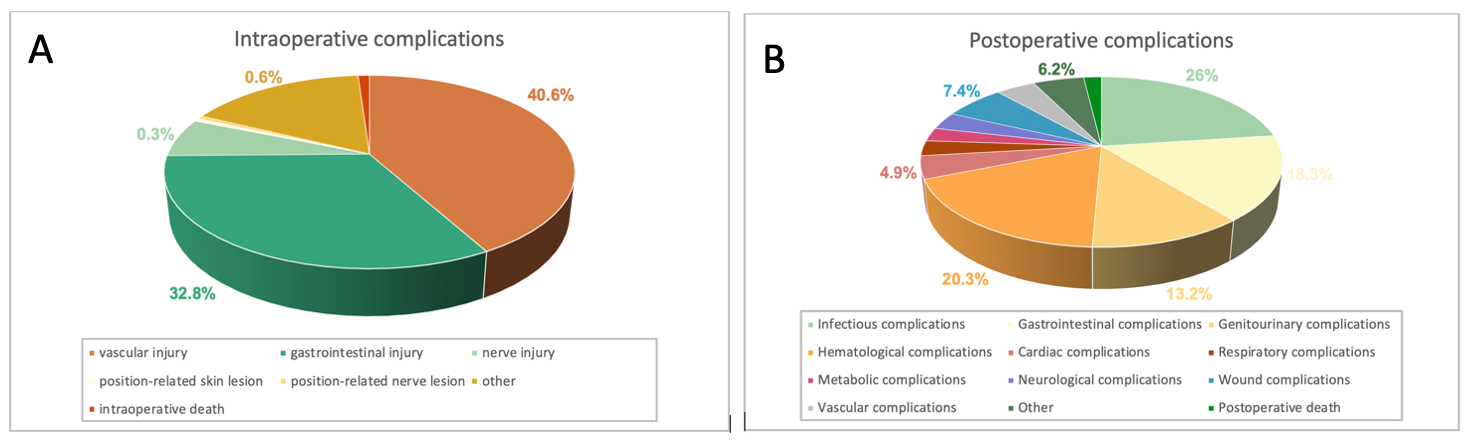
Methods: We retrospectively analyzed data of 4,731 patients treated with RC for BCa among 25 tertiary referral centers between 2001 and 2020. Intra-operative complications included gastrointestinal (GI), vascular, nerve injury, position-related skin and peripheral nerve lesion, and death. Post-operative complications were coded as early ( <30 days) and late (30-90 days) complications, including infectious, GI, genitourinary (GU), hematological, cardiac, wound complications, and death. Multivariable logistic regression models (LGRs) were applied to evaluate independent predictors of intra- and post-operative complications; covariates consisted of demographic features and perioperative outcomes
Results: Open, laparoscopic, and robotic RC were performed in 69.1%, 10.7%, 20.2% of patients, respectively; conversion from robotic to open technique was recorded in 3 patients. Overall, 3.8% of patients experienced intra-operative complications: vascular injury occurred in 40.6% of cases, followed by GI injury (32.8%); intra-operative death occurred in 1.1% of cases (Fig. 1A). Overall, 64.1% of patients experienced post-operative complications (early: 57.6% and late: 17.9%). Infectious complications occurred in 26% of patients, followed by anemia (20.3%), and GI (18.3%) complications. Death due to early and late complications occurred in 1.5% and 0.6% of patients, respectively (Fig. 1B). At multivariable LGMs prior abdominal surgery (odd ratio [OR]: 1.87; p=0.005) and surgeon experience (>250 RC/surgeon: OR: 0.27; p=0.003) were independent predictors of intra-operative complications, while female gender (OR: 0.66; p=0.03), anticoagulant therapy (OR: 2.05; p=0.04), and post-operative transfusions (OR: 4.84; p<0.001) were independent predictors of post-operative complications. Surgical RC technique was not an independent predictor of complication
Conclusions: RC is still burden with an increased rate of perioperative complications. Risk factors for perioperative complications include scarce surgeon experience, prior abdominal surgery, and post-operative transfusions
Source of Funding: None

.jpg)
.jpg)