Back
Poster, Podium & Video Sessions
Best Poster Award
MP23: Bladder Cancer: Invasive III
MP23-14: Reducing Readmissions Following Radical Cystectomy Through Quality Improvement
Saturday, May 14, 2022
8:45 AM – 10:00 AM
Location: Room 225
Lee White*, Caleb Seufert, Stanford, CA, Bogdana Schmidt, Salt Lake City, UT, Peter Dy, Stacy Cox, Mia Singh, Joanne Meneses, Eila Skinner, Stanford, CA
Lee W. White, MD, PHD
Stanford
Poster Presenter(s)
Introduction: Radical cystectomy (RC) for invasive for invasive bladder cancer is a highly morbid surgery. At 21 to 31%, the national 30 day RC readmission rate is significantly higher than for other urologic procedures. Early rehospitalization has become a focus due to the impact on patient experience, high cost, and associated poor downstream health outcomes. Under the auspices of the Stanford Clinical Effectiveness and Leadership Training Program, we set out to reduce the 30-day readmission rate due to infection to 10%, from the current rate at Stanford of 17.9%.
Methods: We determined the baseline readmission rate at Stanford from ACS NSQUIP and billing data, and manual review of all RCs at Stanford from 2018-2020. We identified an ‘intervention bundle’ to reduce cystectomy readmissions: preoperative nutrition referral, enrolling patients in SeamlessMD perioperative education platform, standardized teaching for patients during hospitalization, removal of ureteral stents by postoperative day 4, methenamine urinary tract infection prophylaxis, and outpatient care coordination with followup visit at 3, 10, and 17 days post-discharge.
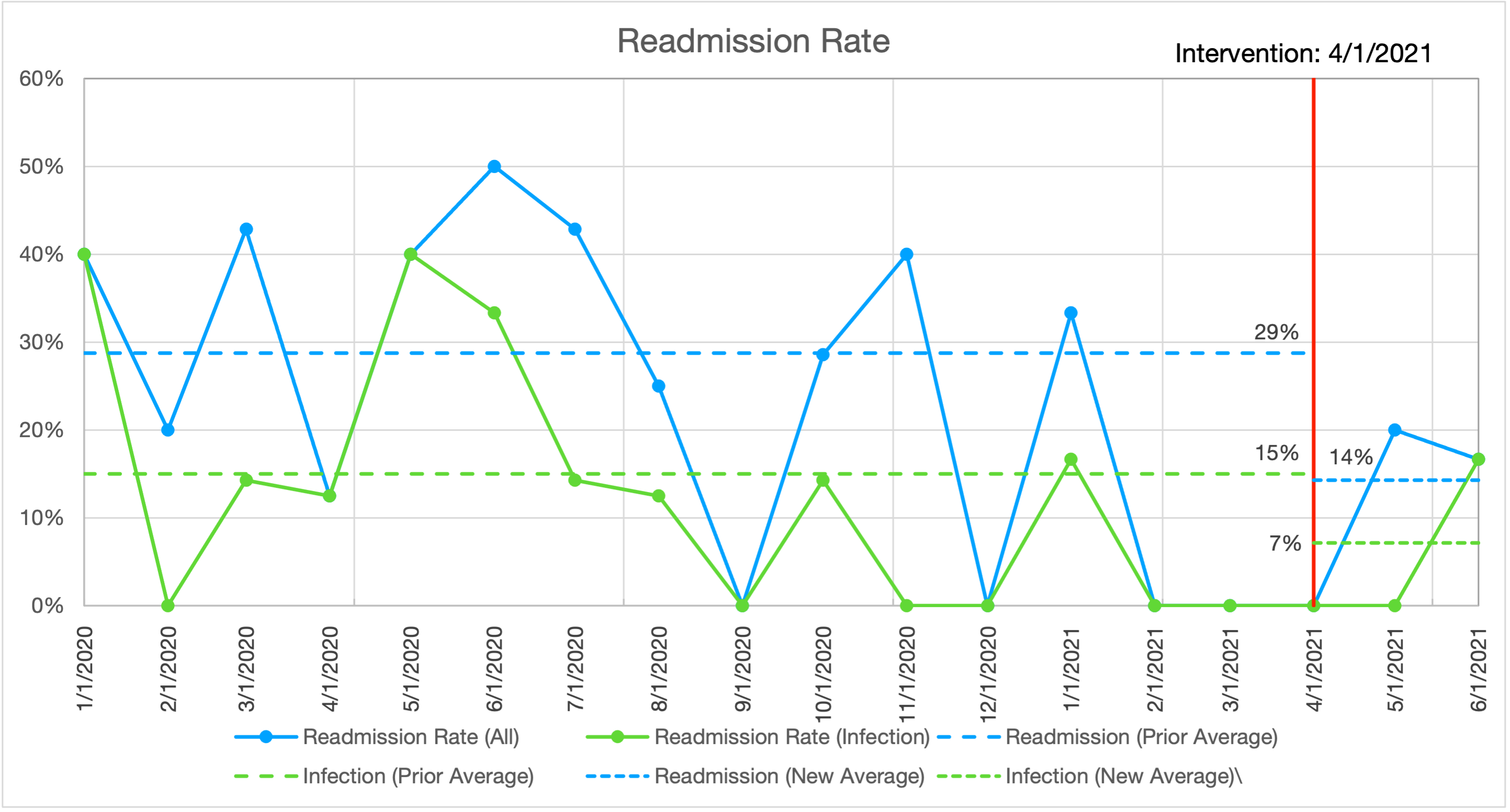
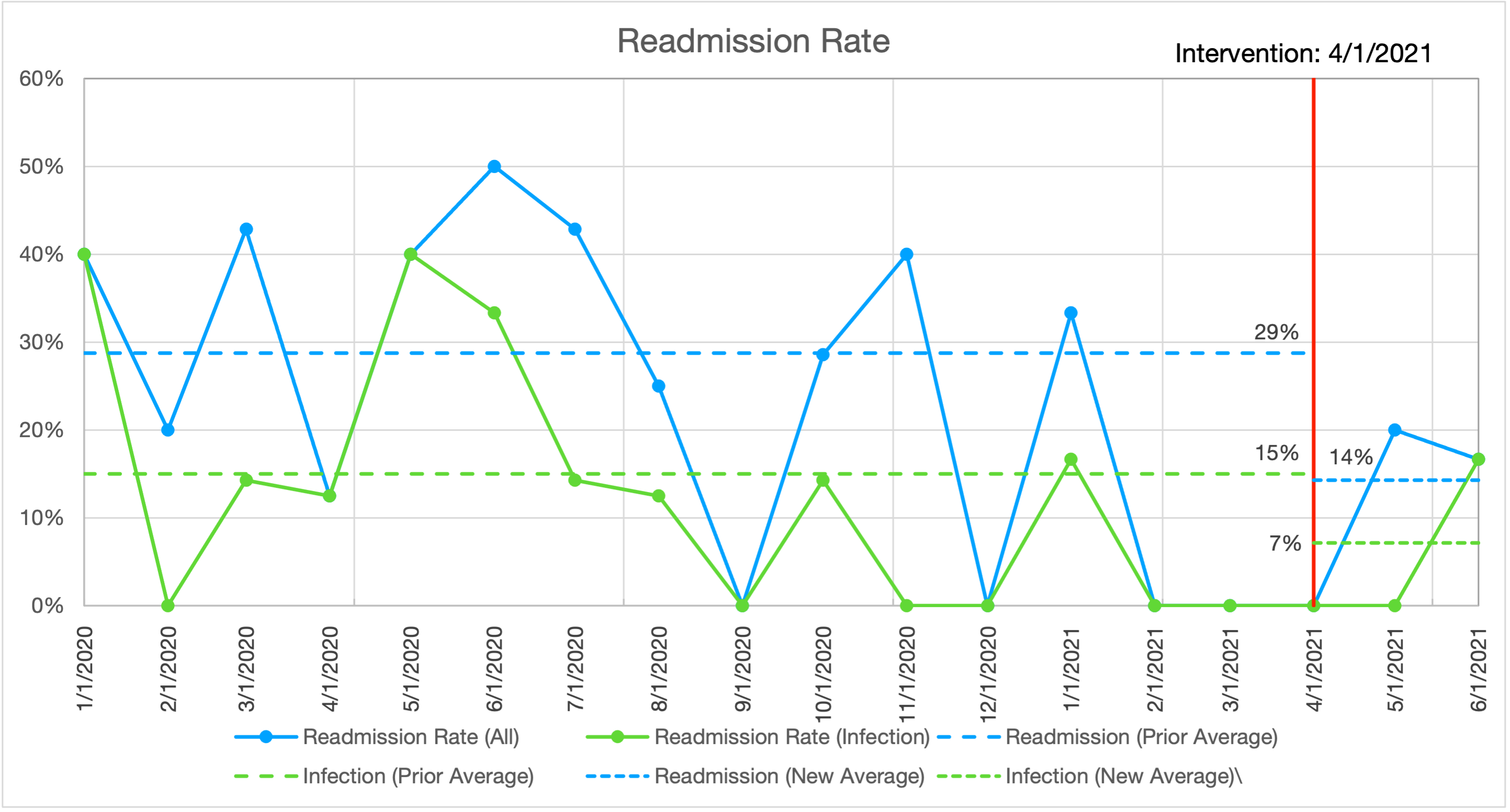
Results: We identified 217 baseline cases from 2018-20 with a readmission rate of 28-32%, of which 18-21% were due to intraabdominal and urinary tract infection. In the 3 months since our intervention, we performed 14 radical cystectomies. 1 patient was admitted to an outside hospital with pain. One patient was admitted with a urinary tract infection. These represent a 14% overall readmission rate and 7% readmission rate for infection. Process measures have also improved. Days to stent removal has improved from 21.3 days to 7.7 days. Days to clinic follow-up improved from 6.3 days to 3.6 days.
Conclusions: Our intervention reduced readmissions from 17.9% to <10%, or an estimated 6-10 prevented readmissions annually, with corresponding impact of $1-1.5M. Insights from this initiative provide a template for improving important clinical metrics using data from chart and literature review. This Quality Improvement initiative included a spectrum of practitioners. Reducing readmission following cystectomy may yield strategies and answers to reduce readmission following other complex and morbid surgeries. These answers can improve the experience for patients at Stanford and beyond.
Source of Funding: NA
Methods: We determined the baseline readmission rate at Stanford from ACS NSQUIP and billing data, and manual review of all RCs at Stanford from 2018-2020. We identified an ‘intervention bundle’ to reduce cystectomy readmissions: preoperative nutrition referral, enrolling patients in SeamlessMD perioperative education platform, standardized teaching for patients during hospitalization, removal of ureteral stents by postoperative day 4, methenamine urinary tract infection prophylaxis, and outpatient care coordination with followup visit at 3, 10, and 17 days post-discharge.
Results: We identified 217 baseline cases from 2018-20 with a readmission rate of 28-32%, of which 18-21% were due to intraabdominal and urinary tract infection. In the 3 months since our intervention, we performed 14 radical cystectomies. 1 patient was admitted to an outside hospital with pain. One patient was admitted with a urinary tract infection. These represent a 14% overall readmission rate and 7% readmission rate for infection. Process measures have also improved. Days to stent removal has improved from 21.3 days to 7.7 days. Days to clinic follow-up improved from 6.3 days to 3.6 days.
Conclusions: Our intervention reduced readmissions from 17.9% to <10%, or an estimated 6-10 prevented readmissions annually, with corresponding impact of $1-1.5M. Insights from this initiative provide a template for improving important clinical metrics using data from chart and literature review. This Quality Improvement initiative included a spectrum of practitioners. Reducing readmission following cystectomy may yield strategies and answers to reduce readmission following other complex and morbid surgeries. These answers can improve the experience for patients at Stanford and beyond.
Source of Funding: NA

.jpg)
.jpg)