Back
Poster, Podium & Video Sessions
Moderated Poster
MP23: Bladder Cancer: Invasive III
MP23-15: Impact of previous treatments for prostate cancer on perioperative and oncological outcomes in patients treated with radical cystectomy for bladder cancer
Saturday, May 14, 2022
8:45 AM – 10:00 AM
Location: Room 225
Stefano Tappero*, Stefano Parodi, Guglielmo Mantica, Marco Borghesi, Genoa, Italy, Cristian Fiori, Matteo Manfredi, Turin, Italy, Marco Bandini, Milan, Italy, Andrea Mari, Francesca Valastro, Florence, Italy, Maria Angela Cerruto, Alessandra Gozzo, Verona, Italy, Francesco Chessa, Riccardo Schiavina, Bologne, Italy, Alberto Briganti, Milan, Italy, Andrea Minervini, Florence, Italy, Alessandro Antonelli, Verona, Italy, Francesco Porpiglia, Turin, Italy, Eugenio Brunocilla, Bologne, Italy, Francesco Montorsi, Milan, Italy, Nazareno Suardi, Carlo Terrone, Genoa, Italy
Stefano Tappero, MD
IRCCS Ospedale Policlinico San Martino
Poster Presenter(s)
Introduction: Radical cystectomy (RC) is technically challenging in patients with history of previous treatments for prostate cancer (ptPCa) and burdened by high complication rates. However, only small series have been reported in this field, and none focused on oncological outcomes. We aimed to assess the impact of ptPCa on the outcomes of RC for bladder cancer (BCa) relying on a large multicentric cohort of ptPCa patients.
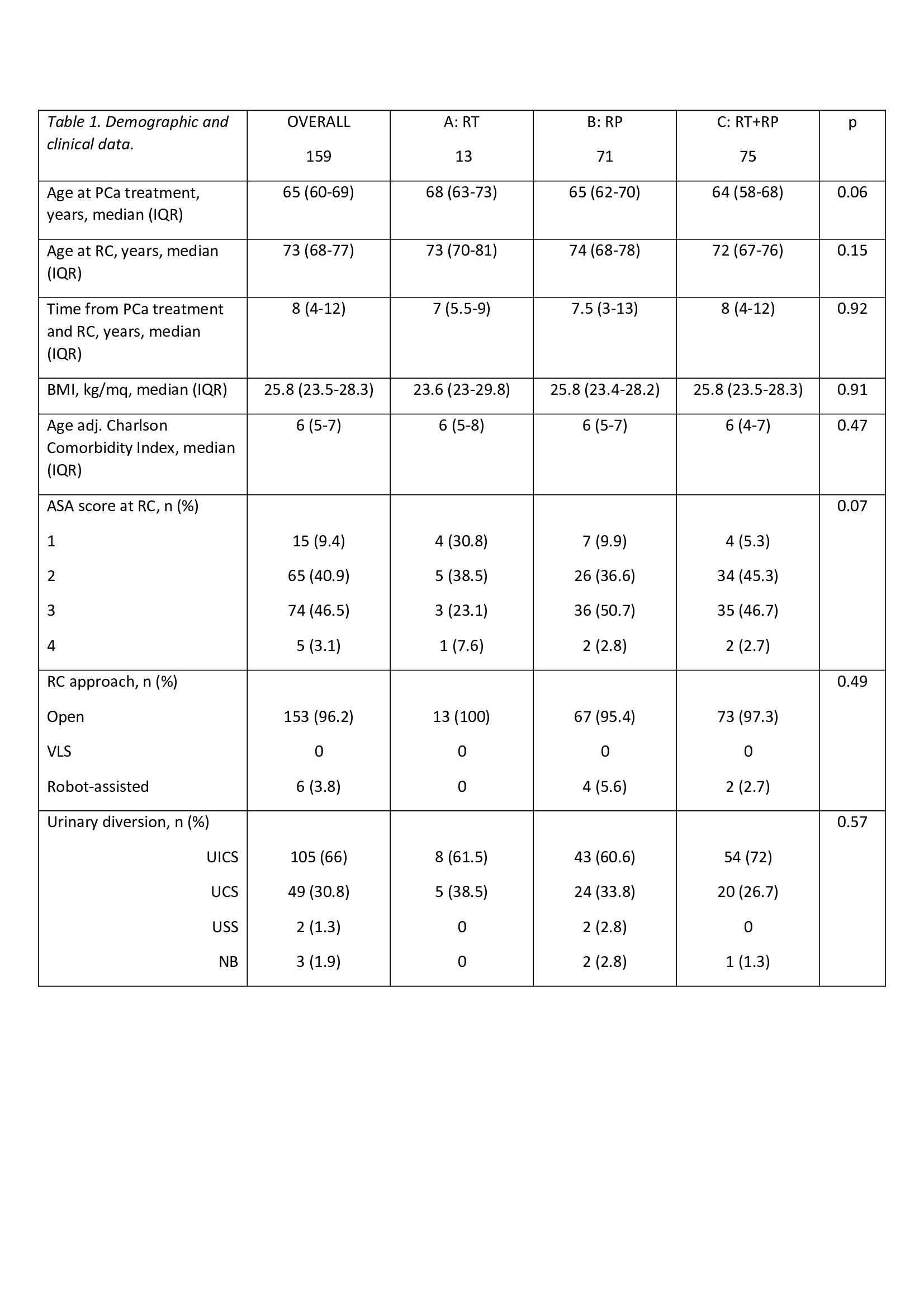
Methods: We analyzed 159 ptPCa patients treated with RC for BCa between 2010 and 2019 at six high-volume Institutions. According to ptPCa we divided patients as follows: previous radiotherapy (RT, Group A: 13), previous radical prostatectomy (RP, Group B: 71) and both RP and either adjuvant or salvage RT (Group C: 75). RC perioperative outcomes and follow-up data were collected. 30-day complications were reported according to the standardized methodology proposed by the EAU guidelines. Kaplan-Meier analyses were used to depict 2-year BCa local recurrence (BCLR), systemic recurrence (BCSR) and specific mortality (BCSM). Cox regression models were used to predict BCLR, BCSR and BCSM according to ptPCa. Covariates consisted of CCI, pT and pN stage.
Results: Table 1 displays clinical and perioperative characteristics of the population. Operative time of RC was longer for patients in group C (p=0.02). No relevant differences were observed in terms of blood loss, intraoperative transfusions, and length of stay. Overall, 93 patients experienced 120 postoperative complications, of whom 95 (79.2%) classified as low grade (Clavien =II) and 25 (20.8%) as high grade (Clavien =III). Group B had the lowest complications rate (52.1% vs. 84.6% in Group A vs. 96% in Group C; p=0.05). Median follow-up was 23 months (IQR 5-46). The 30-mo BCSM-free survival was 89% in group A, 81% in group B and 89% in group C (p=0.26). At multivariable Cox analysis, after adjusting for CCI, pT and pN stage, no previous specific treatment for PCa reached the status of independent predictor of BCLR, BCSR and BCSM (all p>0.2).
Conclusions: In patients submitted to RC for BCa no previous treatment for PCa specifically affects short-term oncological outcomes. A trend towards higher complication rates is observed in previously irradiated patients.
Source of Funding: -
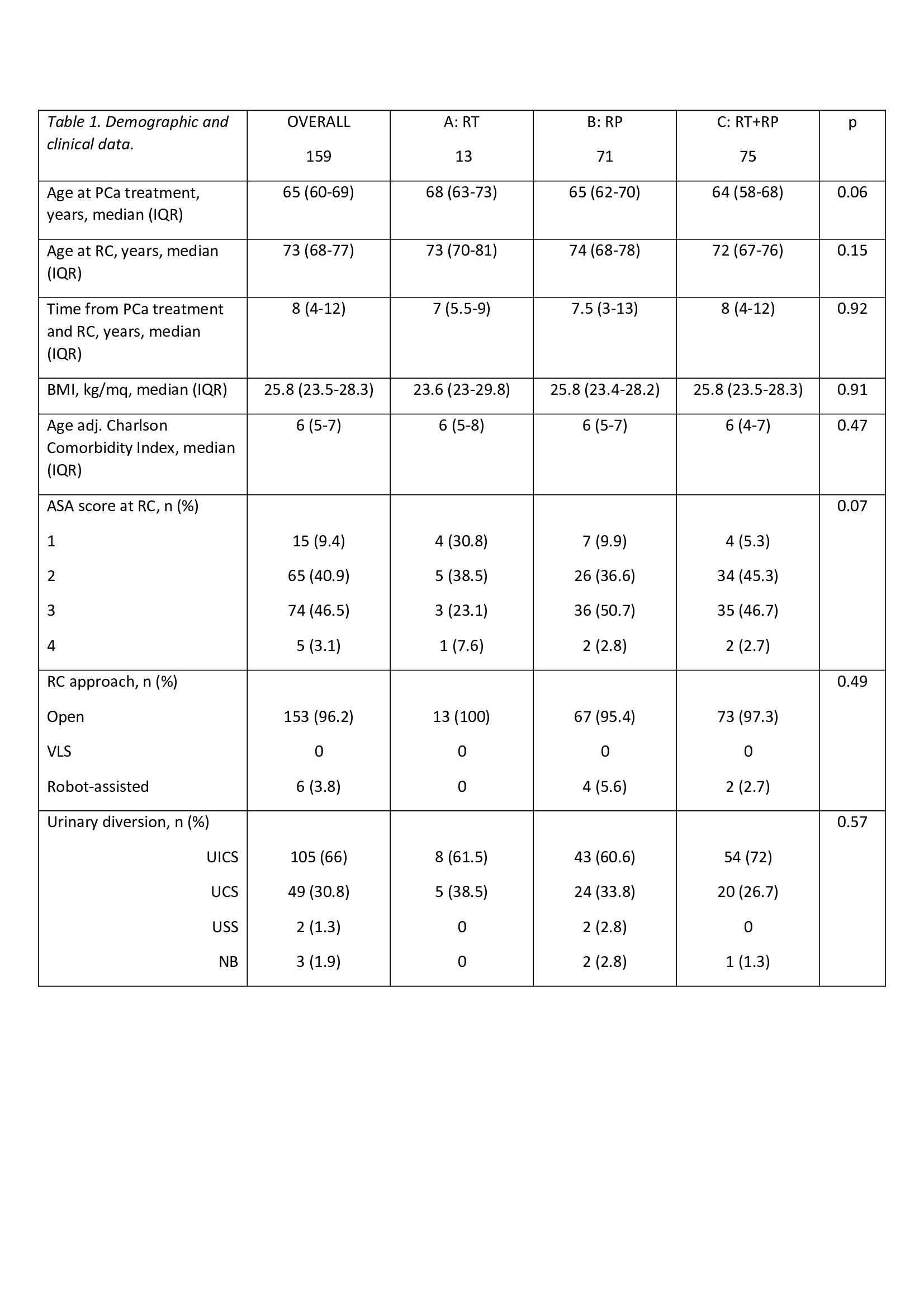
Methods: We analyzed 159 ptPCa patients treated with RC for BCa between 2010 and 2019 at six high-volume Institutions. According to ptPCa we divided patients as follows: previous radiotherapy (RT, Group A: 13), previous radical prostatectomy (RP, Group B: 71) and both RP and either adjuvant or salvage RT (Group C: 75). RC perioperative outcomes and follow-up data were collected. 30-day complications were reported according to the standardized methodology proposed by the EAU guidelines. Kaplan-Meier analyses were used to depict 2-year BCa local recurrence (BCLR), systemic recurrence (BCSR) and specific mortality (BCSM). Cox regression models were used to predict BCLR, BCSR and BCSM according to ptPCa. Covariates consisted of CCI, pT and pN stage.
Results: Table 1 displays clinical and perioperative characteristics of the population. Operative time of RC was longer for patients in group C (p=0.02). No relevant differences were observed in terms of blood loss, intraoperative transfusions, and length of stay. Overall, 93 patients experienced 120 postoperative complications, of whom 95 (79.2%) classified as low grade (Clavien =II) and 25 (20.8%) as high grade (Clavien =III). Group B had the lowest complications rate (52.1% vs. 84.6% in Group A vs. 96% in Group C; p=0.05). Median follow-up was 23 months (IQR 5-46). The 30-mo BCSM-free survival was 89% in group A, 81% in group B and 89% in group C (p=0.26). At multivariable Cox analysis, after adjusting for CCI, pT and pN stage, no previous specific treatment for PCa reached the status of independent predictor of BCLR, BCSR and BCSM (all p>0.2).
Conclusions: In patients submitted to RC for BCa no previous treatment for PCa specifically affects short-term oncological outcomes. A trend towards higher complication rates is observed in previously irradiated patients.
Source of Funding: -

.jpg)
.jpg)