Back
Poster, Podium & Video Sessions
Moderated Poster
MP23: Bladder Cancer: Invasive III
MP23-16: Circulating tumor DNA is a strong predictor in patients treated with systemic therapy for urothelial carcinoma
Saturday, May 14, 2022
8:45 AM – 10:00 AM
Location: Room 225
Ekaterina Laukhtina*, Melanie R. Hassler, Benjamin Pradere, Maximilian Pallauf, David D’Andrea, Vienna, Austria, Dmitry Enikeev, Moscow, Russian Federation, Shahrokh F. Shariat, Vienna, Austria

Ekaterina Laukhtina
Medical University of Vienna
Poster Presenter(s)
Introduction: In patients with urothelial carcinoma (UC), management decisions are mainly based on clinicopathological characteristics. However, there is a need for more accurate prognostic and predictive tools. Previous studies have suggested that circulating tumor DNA (ctDNA) can reflect tumor burden and guide potential therapeutic strategies in several malignancies. This study aimed to summarize the available data and identify the prognostic value of ctDNA in patients treated with systemic therapy for urothelial carcinoma (UC).
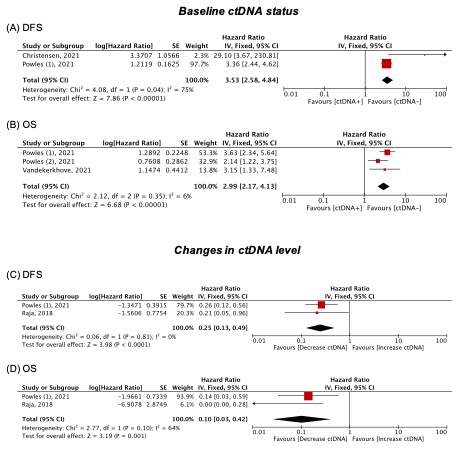
Methods: The MEDLINE and EMBASE databases were searched in October 2021 according to the PRISMA statement. Studies were deemed eligible if they reported on oncologic outcomes in patients treated with systemic therapy for UC based on their ctDNA baseline profile (before the start of the systemic therapy) and/or changes over the course of therapy. The primary outcomes of interest were disease-free survival (DFS) and overall survival (OS). Forest plots were used to assess the hazard ratios (HR) and 95% confidence intervals (95% CIs) to describe the relationships between ctDNA and survival outcomes.
Results: Five studies met the eligibility criteria. Among the included studies, patient populations were highly heterogeneous including some treated with immunotherapy and others with chemotherapy within either the neo/adjuvant or metastatic settings. We found a strong association between high baseline ctDNA levels and worse DFS (HR: 3.53, 95% CI: 2.58–4.84) and OS (HR: 2.99, 95% CI: 2.17–4.13) in UC patients treated with systemic therapy. Patients with decreasing ctDNA level in response to immunotherapy had better DFS (HR: 0.25, 95% CI: 0.13–0.49) and OS (HR: 0.10, 95% CI: 0.03–0.42) compared to their counterparts who did not exhibit a decline in ctDNA.
Conclusions: Our analysis indicates that increased levels of ctDNA are associated with worse survival outcomes in patients treated with systemic therapy for UC. UC patients who exhibit a decrease in ctDNA levels during the course of systemic therapy had better survival outcomes compared to those with stable or increasing ctDNA levels. While promising, the role of ctDNA as an adjunct to established histopathologic characteristics for clinical decision-making requires further validation as part of the biomarker phased approach.
Source of Funding: None.
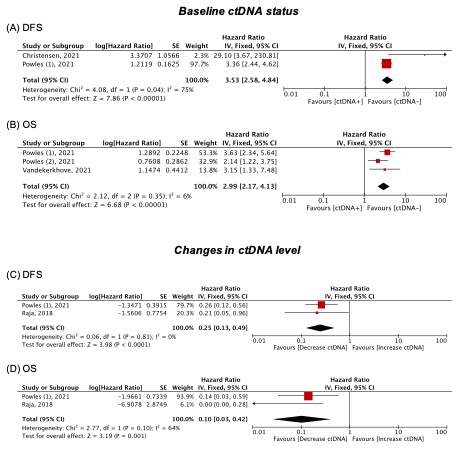
Methods: The MEDLINE and EMBASE databases were searched in October 2021 according to the PRISMA statement. Studies were deemed eligible if they reported on oncologic outcomes in patients treated with systemic therapy for UC based on their ctDNA baseline profile (before the start of the systemic therapy) and/or changes over the course of therapy. The primary outcomes of interest were disease-free survival (DFS) and overall survival (OS). Forest plots were used to assess the hazard ratios (HR) and 95% confidence intervals (95% CIs) to describe the relationships between ctDNA and survival outcomes.
Results: Five studies met the eligibility criteria. Among the included studies, patient populations were highly heterogeneous including some treated with immunotherapy and others with chemotherapy within either the neo/adjuvant or metastatic settings. We found a strong association between high baseline ctDNA levels and worse DFS (HR: 3.53, 95% CI: 2.58–4.84) and OS (HR: 2.99, 95% CI: 2.17–4.13) in UC patients treated with systemic therapy. Patients with decreasing ctDNA level in response to immunotherapy had better DFS (HR: 0.25, 95% CI: 0.13–0.49) and OS (HR: 0.10, 95% CI: 0.03–0.42) compared to their counterparts who did not exhibit a decline in ctDNA.
Conclusions: Our analysis indicates that increased levels of ctDNA are associated with worse survival outcomes in patients treated with systemic therapy for UC. UC patients who exhibit a decrease in ctDNA levels during the course of systemic therapy had better survival outcomes compared to those with stable or increasing ctDNA levels. While promising, the role of ctDNA as an adjunct to established histopathologic characteristics for clinical decision-making requires further validation as part of the biomarker phased approach.
Source of Funding: None.

.jpg)
.jpg)