Back
Poster, Podium & Video Sessions
Moderated Poster
MP24: Kidney Cancer: Localized: Surgical Therapy I
MP24-03: Local recurrence following partial nephrectomy in patients with renal cell carcinoma: a multicenter study
Saturday, May 14, 2022
8:45 AM – 10:00 AM
Location: Room 222
Shohei Fukuda*, Hajime Tanaka, Kenji Tanabe, Tokyo, Japan, Takashi Tamiya, Saitama, Japan, Masaki Kobayashi, Tokyo, Japan, Shugo Yajima, Chiba, Japan, Yuki Nakamura, Saitama, Japan, Motohiro Fujiwara, Tokyo, Japan, Yudai Ishikawa, Ibaraki, Japan, Takanobu Yamamoto, Tokyo, Japan, Saori Araki, Chiba, Japan, Soichiro Yoshida, Minato Yokoyama, Yoh Matsuoka, Yukihiro Otsuka, Fumitaka Koga, Yasuhisa Fujii, Tokyo, Japan
- SF
Shohei Fukuda, MD
Tokyo Medical and Dental University
Poster Presenter(s)
Introduction: Partial nephrectomy (PN) is a standard surgical treatment for small renal masses and yields favorable functional and oncological outcomes. To date, studies assessing clinical characteristics of local recurrence following PN have been relatively sparse. We investigated the incidence and risk factors for local recurrence after PN and also evaluated the prognosis of patients who developed local recurrence.
Methods: This multicenter retrospective study included 1568 renal cell carcinoma (RCC) patients who underwent PN for a solitary renal tumor from 1991 to 2019 (approval number, M2019-172). Local recurrence after PN was defined as detection of a new recurrent lesion in the ipsilateral renal parenchyma or perinephric fat. We analyzed the patients’ characteristics and tumor factors that were associated with local recurrence. Clinical courses of patients with local recurrence following PN were also reviewed.
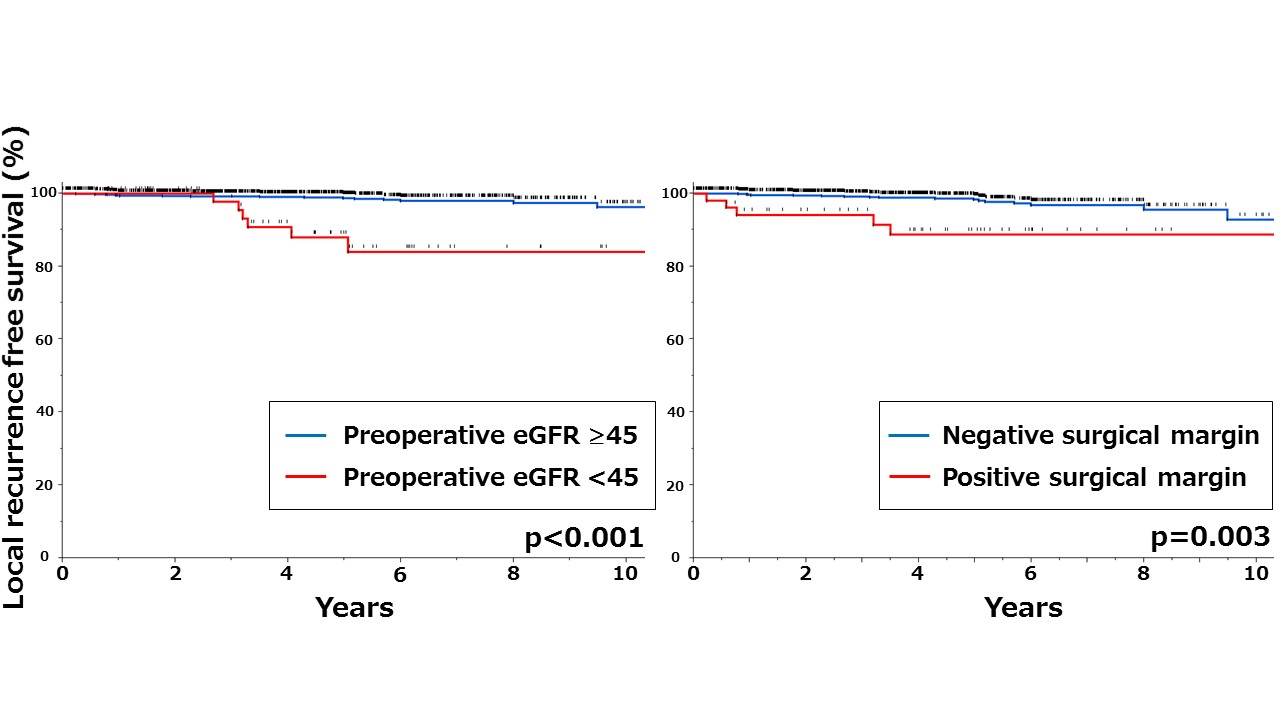
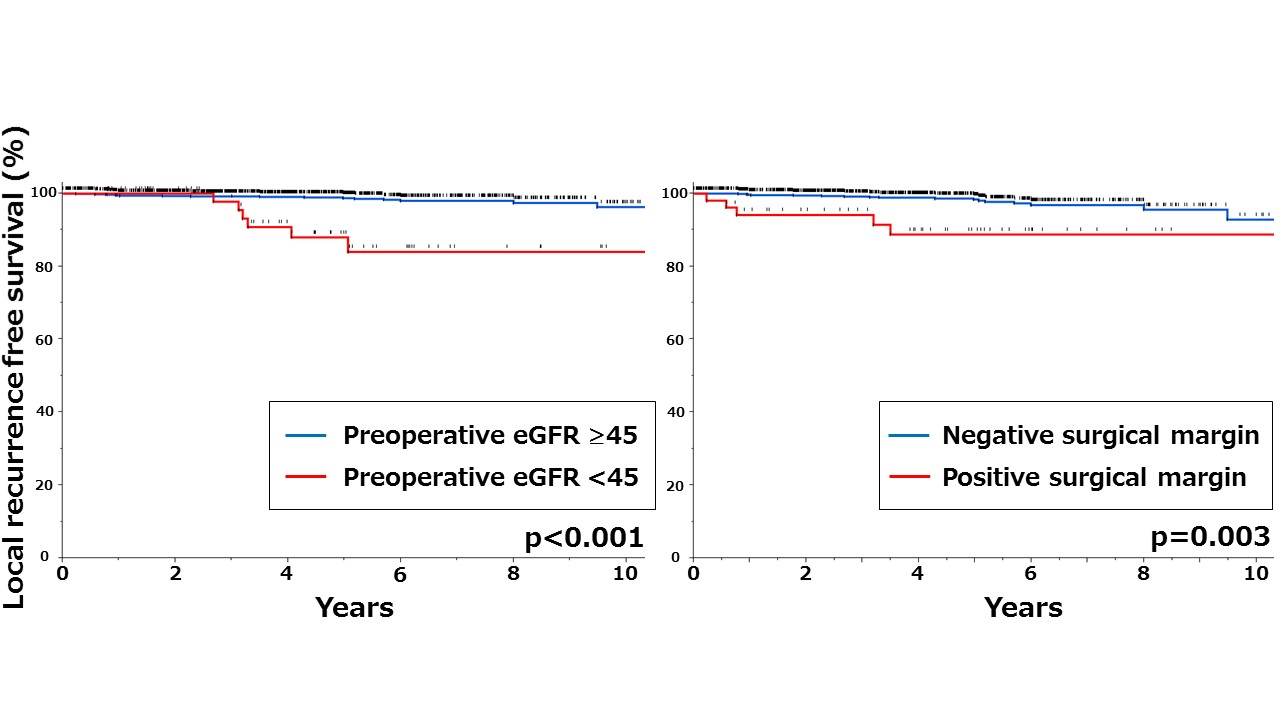
Results: The median age was 62 years and 1176 (75%) patients were male. Preoperative eGFR was 72 ml/min/1.73m2 and 74 (4.7%) patients had preoperative renal impairment (eGFR <45 mL/min/1.73 m2). The median tumor size was 2.7 cm and the median R.E.N.A.L nephrometry score was 7. A majority of patients were diagnosed with clear cell RCC (85%, n=1331) and pathological T1a tumor (88%, n=1384). Positive surgical margin was detected in 54 (3.4%) patients. During a median follow-up period of 52 months, 62 (4.0%) patients developed distant metastases and 14 (0.9%) patients died of RCC. A total of 28 (1.8%) patients developed local recurrence and the median time to local recurrence from PN was 45 months. Multivariable analysis identified preoperative renal impairment (eGFR <45) and positive surgical margin as significant risk factors for local recurrence (p = 0.004 and p = 0.002, respectively). Among 28 patients with local recurrence, 10 (36%) patients developed distant metastases concurrently or subsequently as well and one (3.6%) patient died of RCC. Sixteen (57%) patients underwent surgery (n=14) or percutaneous ablation (n=2) for local recurrence and 14 (50%) patients achieved disease free survival.
Conclusions: Preoperative renal impairment and positive surgical margin were associated with local recurrence following PN. Patients who were able to undergo local treatment for local recurrence showed favorable prognosis.
Source of Funding: none
Methods: This multicenter retrospective study included 1568 renal cell carcinoma (RCC) patients who underwent PN for a solitary renal tumor from 1991 to 2019 (approval number, M2019-172). Local recurrence after PN was defined as detection of a new recurrent lesion in the ipsilateral renal parenchyma or perinephric fat. We analyzed the patients’ characteristics and tumor factors that were associated with local recurrence. Clinical courses of patients with local recurrence following PN were also reviewed.
Results: The median age was 62 years and 1176 (75%) patients were male. Preoperative eGFR was 72 ml/min/1.73m2 and 74 (4.7%) patients had preoperative renal impairment (eGFR <45 mL/min/1.73 m2). The median tumor size was 2.7 cm and the median R.E.N.A.L nephrometry score was 7. A majority of patients were diagnosed with clear cell RCC (85%, n=1331) and pathological T1a tumor (88%, n=1384). Positive surgical margin was detected in 54 (3.4%) patients. During a median follow-up period of 52 months, 62 (4.0%) patients developed distant metastases and 14 (0.9%) patients died of RCC. A total of 28 (1.8%) patients developed local recurrence and the median time to local recurrence from PN was 45 months. Multivariable analysis identified preoperative renal impairment (eGFR <45) and positive surgical margin as significant risk factors for local recurrence (p = 0.004 and p = 0.002, respectively). Among 28 patients with local recurrence, 10 (36%) patients developed distant metastases concurrently or subsequently as well and one (3.6%) patient died of RCC. Sixteen (57%) patients underwent surgery (n=14) or percutaneous ablation (n=2) for local recurrence and 14 (50%) patients achieved disease free survival.
Conclusions: Preoperative renal impairment and positive surgical margin were associated with local recurrence following PN. Patients who were able to undergo local treatment for local recurrence showed favorable prognosis.
Source of Funding: none

.jpg)
.jpg)