Back
Poster, Podium & Video Sessions
Moderated Poster
MP24: Kidney Cancer: Localized: Surgical Therapy I
MP24-05: Outcomes of partial nephrectomy for non-metastatic cT2 renal tumors: results from a Canadian multi-institutional collaborative
Saturday, May 14, 2022
8:45 AM – 10:00 AM
Location: Room 222
Rahul Bansal*, Ryan Sun, Winnipeg, Canada, Frederic Pouliot, Quebec City, Canada, Ranjeeta Mallick, Ottawa, Canada, Simon Tanguay, Montreal, Canada, Darrel Drachenberg, Winnipeg, Canada, Richard Rendon, Halifax, Canada, Alan So, Vancouver, Canada, Luke Lavallee, Ottawa, Canada, Antonio Finelli, Toronto, Canada, Lucas Dean, Edmonton, Canada, Anil Kapoor, Hamilton, Canada, Bimal Bhindi, Calgary, Canada, Lori Wood, Halifax, Canada, Naveen Basappa, Edmonton, Canada, Rodney Breau, Ottawa, Canada
Poster Presenter(s)
Introduction: The role of PN is not well defined for cT2 renal cell carcinoma (RCC) as compared to radical nephrectomy (RN). The aim of this study was to examine oncological outcomes of PN as compared to RN for non-metastatic cT2 RCC.
Methods: The Canadian Kidney Cancer information system was used to define patients who underwent surgery for non-metastatic cT2 RCC from January 2011 to October 2021. Patients with clear-cell, papillary, and chromophobe RCC were included. Other histology, multiple tumours, and hereditary RCC syndrome patients were excluded. Each PN patient was individually matched to RN up to 1:4 depending on availability of patients based on tumor size (+/- 1cm), histology, grade (clear cell and papillary), and necrosis (clear cell). Matched patients were analyzed as clusters.
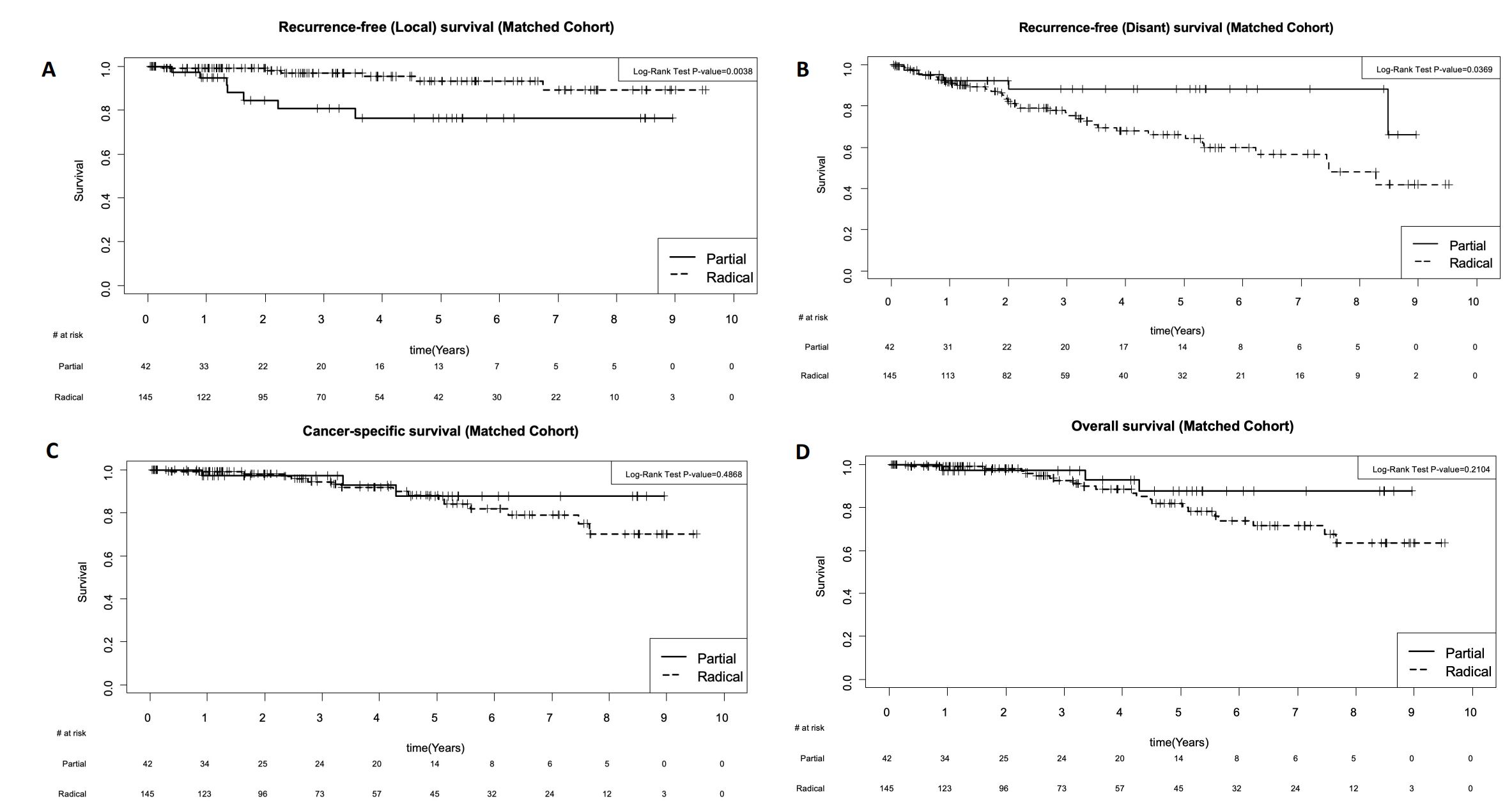
Results: A total of 1347 patients were identified, and 42 PN patients met study criteria who were then matched to 145 RN patients. Both groups had similar age, gender, smoking status, BMI, Charlson comorbidity index score, symptoms at presentation, baseline eGFR, hemoglobin and pathological characteristics. PN patients had smaller tumors (7.6 cm [IQR 7.2, 9.2] vs. (8.5 cm [IQR 7.6, 10.3], p = 0.048), had higher likelihood of undergoing open surgery (75% vs. 30% p<0.0001), less likely received adrenalectomy (0 vs. 21%, p=0.0001) and had higher likelihood of positive surgical margin (PSM) (10% vs. 1%, p = 0.025). Median follow up was not significantly different in either group (3.7yrs [IQR 1.1, 5.4] in PN vs. 2.8yrs [IQR 1.2, 5.6] in RN, p=0.79). During the follow up period, PN patients had higher risk of local recurrence (HR 4.38 95% CI 1.51-12.71) and lower risk of metastasis (HR 0.39; 95% CI 0.16-0.95), improved cancer specific survival (HR 0.65; 95% CI 0.22-1.87) and overall survival (HR 0.47; 0.17-1.27) as compared to RN (Fig.1).
Conclusions: In this multi-institutional Canadian cohort of patients with non-metastatic cT2 RCC undergoing surgery, PN was associated with higher likelihood of PSM and local recurrence as compared to RN and lower risk of distant metastasis, cancer related death or death from any cause. Despite individual patient matching, there is likely unadjusted selection bias resulting in superior cancer survival associated with PN.
Source of Funding: N/A
Methods: The Canadian Kidney Cancer information system was used to define patients who underwent surgery for non-metastatic cT2 RCC from January 2011 to October 2021. Patients with clear-cell, papillary, and chromophobe RCC were included. Other histology, multiple tumours, and hereditary RCC syndrome patients were excluded. Each PN patient was individually matched to RN up to 1:4 depending on availability of patients based on tumor size (+/- 1cm), histology, grade (clear cell and papillary), and necrosis (clear cell). Matched patients were analyzed as clusters.
Results: A total of 1347 patients were identified, and 42 PN patients met study criteria who were then matched to 145 RN patients. Both groups had similar age, gender, smoking status, BMI, Charlson comorbidity index score, symptoms at presentation, baseline eGFR, hemoglobin and pathological characteristics. PN patients had smaller tumors (7.6 cm [IQR 7.2, 9.2] vs. (8.5 cm [IQR 7.6, 10.3], p = 0.048), had higher likelihood of undergoing open surgery (75% vs. 30% p<0.0001), less likely received adrenalectomy (0 vs. 21%, p=0.0001) and had higher likelihood of positive surgical margin (PSM) (10% vs. 1%, p = 0.025). Median follow up was not significantly different in either group (3.7yrs [IQR 1.1, 5.4] in PN vs. 2.8yrs [IQR 1.2, 5.6] in RN, p=0.79). During the follow up period, PN patients had higher risk of local recurrence (HR 4.38 95% CI 1.51-12.71) and lower risk of metastasis (HR 0.39; 95% CI 0.16-0.95), improved cancer specific survival (HR 0.65; 95% CI 0.22-1.87) and overall survival (HR 0.47; 0.17-1.27) as compared to RN (Fig.1).
Conclusions: In this multi-institutional Canadian cohort of patients with non-metastatic cT2 RCC undergoing surgery, PN was associated with higher likelihood of PSM and local recurrence as compared to RN and lower risk of distant metastasis, cancer related death or death from any cause. Despite individual patient matching, there is likely unadjusted selection bias resulting in superior cancer survival associated with PN.
Source of Funding: N/A

.jpg)
.jpg)
