Back
Poster, Podium & Video Sessions
Moderated Poster
MP24: Kidney Cancer: Localized: Surgical Therapy I
MP24-07: Adverse Radiologic and Pathologic Features Impact Survival Outcomes for Small Renal Masses Following Nephrectomy
Saturday, May 14, 2022
8:45 AM – 10:00 AM
Location: Room 222
Sari Khaleel*, Hong Truong, Song Jiang, Benjamin Davelman, Jonathan Coleman, Ari Hakimi, Paul Russo, New York, NY
Sari S. Khaleel, MD, MSC
MSKCC
Poster Presenter(s)
Introduction: While most small renal masses (SRMs, < 4cm) have excellent prognosis following extirpative treatment, the impact of finding adverse preoperative radiologic and/or postoperative pathologic T3 features in SRMs that undergo partial (PN) or radical nephrectomy (RN) remains unclear. We sought to review clinical outcomes for SRMs that underwent RN/PN at our institution, comparing pT3 SRMs that presented with adverse (T3) preoperative radiologic features (cT3/pT3) to SRMs that had no adverse preoperative radiologic features, with/without subsequent upstaging to pT3 disease (cT1a/pT3 and cT1a/non-pT3, respectively).
Methods: We retrospectively reviewed SRM cases that underwent RN/PN at our institution between 2010-2020, classifying them into one of the three above groups, excluding cases with known advanced (pT4, M1) disease preoperatively. Continuous and categorical variables were compared using ANOVA and Kruskal-Wallis (K-W) tests, respectively. Cox proportional hazard regression (CPHR) analysis was used to model survival outcomes against the presence of adverse pathologic and radiologic features. Analyses were performed using R Statistical Package (v4.04).
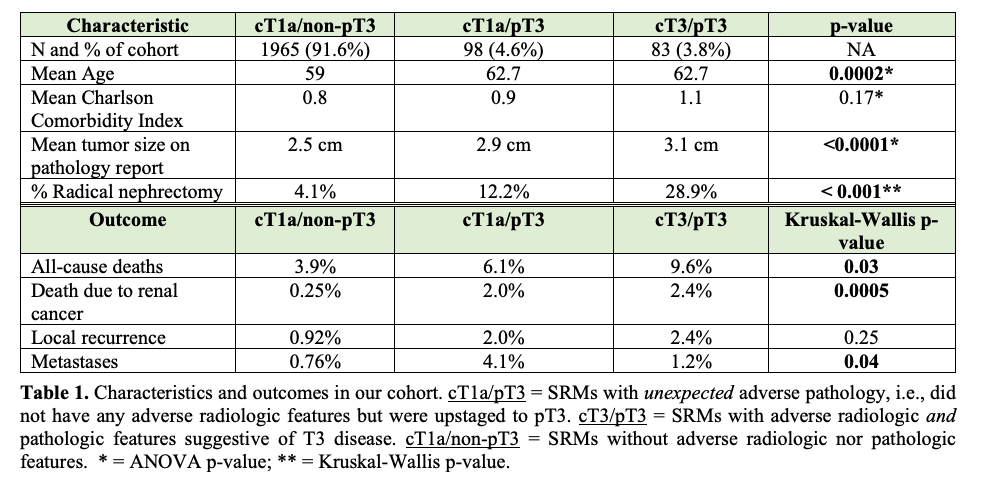
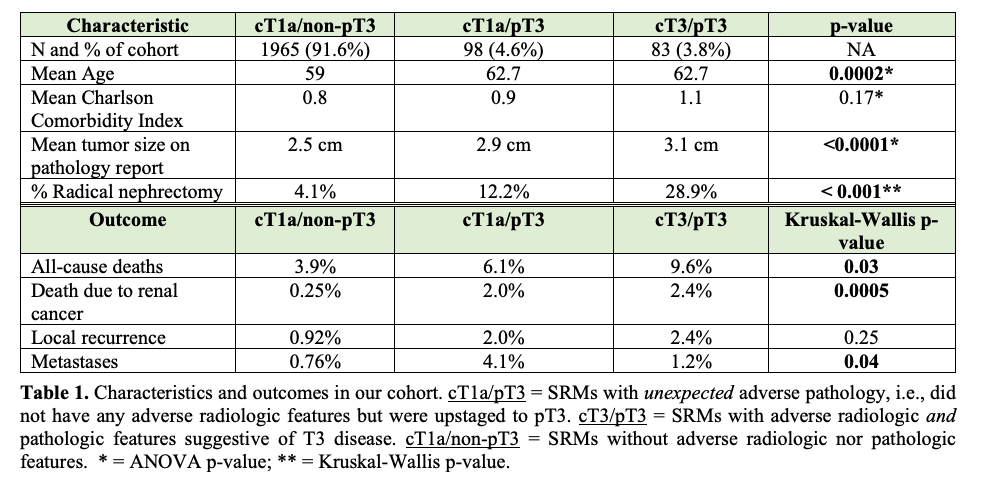
Results: Of 2146 cases, 8.4% were pT3 post-operatively, of which 45.9% had adverse preoperative cT3 radiologic features (Table 1). Median follow-up was 3.3 years (IQR 1.5–6.1). pT3-SRMs had higher rates of radical nephrectomy, positive margins, overall and cancer-specific mortality, and metastases than their non-pT3 counterparts, particularly in the cT3/pT3 subgroup (K-W p< 0.05; Table 1). On multivariate CPHR analysis, only the combined presence of adverse radiologic and pathologic features (cT3/pT3 group) was significantly associated with higher risk for overall- and cancer-specific survival (p < 0.05), adjusting for patient age, BMI, mass size, histology, and Charlson comorbidity index. Unexpected upstaging (cT1a/pT3) was not associated with higher risk of any of the outcomes of interest (p > 0.05).
Conclusions: Adverse pathologic T3 features portend worse outcomes for SRMs, particularly in those with adverse preoperative radiologic features. This study highlights the importance of SRM substratification by these features, which may aid in surgical planning and potential multimodal treatment.
Source of Funding: None
Methods: We retrospectively reviewed SRM cases that underwent RN/PN at our institution between 2010-2020, classifying them into one of the three above groups, excluding cases with known advanced (pT4, M1) disease preoperatively. Continuous and categorical variables were compared using ANOVA and Kruskal-Wallis (K-W) tests, respectively. Cox proportional hazard regression (CPHR) analysis was used to model survival outcomes against the presence of adverse pathologic and radiologic features. Analyses were performed using R Statistical Package (v4.04).
Results: Of 2146 cases, 8.4% were pT3 post-operatively, of which 45.9% had adverse preoperative cT3 radiologic features (Table 1). Median follow-up was 3.3 years (IQR 1.5–6.1). pT3-SRMs had higher rates of radical nephrectomy, positive margins, overall and cancer-specific mortality, and metastases than their non-pT3 counterparts, particularly in the cT3/pT3 subgroup (K-W p< 0.05; Table 1). On multivariate CPHR analysis, only the combined presence of adverse radiologic and pathologic features (cT3/pT3 group) was significantly associated with higher risk for overall- and cancer-specific survival (p < 0.05), adjusting for patient age, BMI, mass size, histology, and Charlson comorbidity index. Unexpected upstaging (cT1a/pT3) was not associated with higher risk of any of the outcomes of interest (p > 0.05).
Conclusions: Adverse pathologic T3 features portend worse outcomes for SRMs, particularly in those with adverse preoperative radiologic features. This study highlights the importance of SRM substratification by these features, which may aid in surgical planning and potential multimodal treatment.
Source of Funding: None

.jpg)
.jpg)