Back
Poster, Podium & Video Sessions
Moderated Poster
MP24: Kidney Cancer: Localized: Surgical Therapy I
MP24-11: Is Pathological Upstaging to T3 Renal Cell Carcinoma Associated with a Similar Prognosis to Non-Upstaged Pathologic T3 Disease? A Multicenter Analysis
Saturday, May 14, 2022
8:45 AM – 10:00 AM
Location: Room 222
Ryan Nasseri*, Kevin Hakimi, Ava Saidian, San Diego, CA, Riccardo Autorino, Richmond, VA, Brian Lane, Grand Rapids, MI, Yasuha Fujii, Tokyo, Japan, Michele Marchioni, Chieti, Italy, Hajime Tanaka, Tokyo, Japan, Dattatraya Patil, Atlanta, GA, Francesco Porpiglia, Torino, Italy, Sabrina Noyes, Grand Rapids, MI, Chandru Sundaram, Indianapolis, IN, James Porter, Seattle, WA, Andrea Minervini, Florence, Italy, Umberto Capitianio, Francesco Montorsi, Milan, Italy, Viraj Master, Atlanta, GA, Ithaar Derweesh, San Diego, CA
- RN
Poster Presenter(s)
Introduction: Pathological upstaging to T3a disease may occur following radical (RN) or partial nephrectomy (PN) for patients with T1/T2 renal cell carcinoma (RCC). Follow up and perceived prognosis for these patients is similar to those who initially presented with clinical T3 RCC. We sought to compare survival outcomes in patients who underwent surgical therapy for upstaged versus non-upstaged pT3 RCC.
Methods: We conducted a retrospective analysis of a multi-institutional dataset of patients who underwent radical (RN) or partial nephrectomy (PN) with final pathologic stage of pT3. Patients were classified as being upstaged (US) from cT1 or cT2 or non-upstaged (NUS) with cT3 disease. Primary outcome was cancer specific survival (CSS)/cancer specific mortality (CSM), with secondary outcomes being Overall Survival (OS)/all-cause mortality (ACM) and Progression/ progression-free survival (PFS). Multivariable Cox regression analysis (MVA) was conducted for predictors of mortality outcomes and Kaplan Meier Analyses (KMA) were conducted for survival outcomes comparing US and NUS groups.
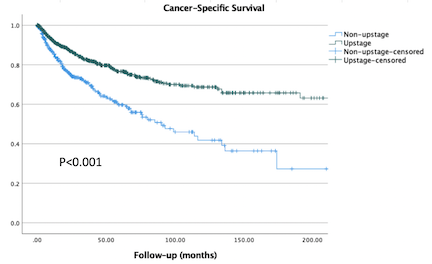
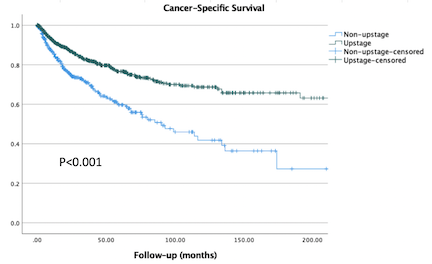
Results: 1232 patients were analyzed (853 US/379 NUS; median follow up 46.2 months). MVA for CSM found that clear cell RCC (HR 2.1, p<0.001), positive surgical margin (HR 1.7, p=0.047), and NUS (HR 1.5, p=0.003) were independently associated with worsened CSM. MVA for ACM revealed age (HR 1.01, p=0.002), RN (HR 2.5, p<0.001), preoperative GFR <60 (HR 1.4, p=0.007), clear-cell RCC (HR 1.4, p=0.007), positive surgical margin (HR 2.2, p<0.001), and NUS (1.27, p=0.023) were independently associated with worsened ACM. MVA for Progression revealed Age (HR 1.01, p=0.022), positive margin (HR 1.9, p=0.016), and NUS (HR 1.67, p<0.001) to be predictive. Comparing NUS and US groups, KMA revealed worsened 5 year CSS (56% vs. 75%, p<0.001; Figure), 5 year OS (42% vs. 58%, p<0.001) and 5 year PFS (33% vs. 58%, p<0.001).
Conclusions: Pathologic upstaging of clinical T1/T2 to T3 RCC was associated with improved survival outcomes when compared to non-upstaged pathologic T3 RCC. Such differences need to be taken into account when designing follow up protocols and for refinement of risk stratification in the T3 RCC stage group. Further investigation is requisite.
Source of Funding: Stephen Weissman Kidney Cancer Research Fund
Methods: We conducted a retrospective analysis of a multi-institutional dataset of patients who underwent radical (RN) or partial nephrectomy (PN) with final pathologic stage of pT3. Patients were classified as being upstaged (US) from cT1 or cT2 or non-upstaged (NUS) with cT3 disease. Primary outcome was cancer specific survival (CSS)/cancer specific mortality (CSM), with secondary outcomes being Overall Survival (OS)/all-cause mortality (ACM) and Progression/ progression-free survival (PFS). Multivariable Cox regression analysis (MVA) was conducted for predictors of mortality outcomes and Kaplan Meier Analyses (KMA) were conducted for survival outcomes comparing US and NUS groups.
Results: 1232 patients were analyzed (853 US/379 NUS; median follow up 46.2 months). MVA for CSM found that clear cell RCC (HR 2.1, p<0.001), positive surgical margin (HR 1.7, p=0.047), and NUS (HR 1.5, p=0.003) were independently associated with worsened CSM. MVA for ACM revealed age (HR 1.01, p=0.002), RN (HR 2.5, p<0.001), preoperative GFR <60 (HR 1.4, p=0.007), clear-cell RCC (HR 1.4, p=0.007), positive surgical margin (HR 2.2, p<0.001), and NUS (1.27, p=0.023) were independently associated with worsened ACM. MVA for Progression revealed Age (HR 1.01, p=0.022), positive margin (HR 1.9, p=0.016), and NUS (HR 1.67, p<0.001) to be predictive. Comparing NUS and US groups, KMA revealed worsened 5 year CSS (56% vs. 75%, p<0.001; Figure), 5 year OS (42% vs. 58%, p<0.001) and 5 year PFS (33% vs. 58%, p<0.001).
Conclusions: Pathologic upstaging of clinical T1/T2 to T3 RCC was associated with improved survival outcomes when compared to non-upstaged pathologic T3 RCC. Such differences need to be taken into account when designing follow up protocols and for refinement of risk stratification in the T3 RCC stage group. Further investigation is requisite.
Source of Funding: Stephen Weissman Kidney Cancer Research Fund

.jpg)
.jpg)