Back
Poster, Podium & Video Sessions
Moderated Poster
MP24: Kidney Cancer: Localized: Surgical Therapy I
MP24-13: Impact of Primary Tumor Size on Cancer-Specific and All-Cause Mortality in Patients Undergoing Cytoreductive Nephrectomy for Metastatic Renal Cell Carcinoma: Analysis from the INternational Marker Consortium for Renal Cancer [INMARC]
Saturday, May 14, 2022
8:45 AM – 10:00 AM
Location: Room 222
Ryan Nasseri*, San Diego, CA, Viraj Master, Atlanta, GA, Yasuhisa Fujii, Tokyo, Japan, Margaret Meagher, Kevin Hakimi, Ava Saidian, San Diego, CA, Dattatraya Patil, Atlanta, GA, Kazutaka Saito, Tokyo, Japan, Ithaar Derweesh, San Diego, CA
- RN
Poster Presenter(s)
Introduction: Management of metastatic Renal Cell Carcinoma (mRCC) is in the process of a dramatic evolution with the a proliferation of systemic agents and reassessment of the role of cytoreductive surgery. The immunological impact of cytoreduction of the primary tumor on systemic disease has long been recognized by the phenomenon of spontaneous regression of distant metastases. We sought to investigate the impact of commonly considered clinical and histologic features on survival outcomes following cytoreductive nephrectomy (CN) for mRCC.
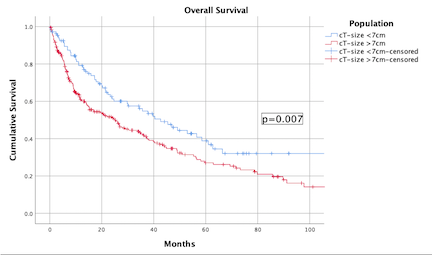
Methods: We performed a multicenter, retrospective analysis using the International Marker Consortium for Renal Cancer (INMARC) identified patients who received CN and systemic therapy from 2001-2019. Demographic and clinical disease factors were analyzed using multivariable Cox regression. KKaplan Meier Analyses (KMA) were conducted to elucidate survival outcomes. Primary outcome was cancer-specific mortality (CSM), secondary outcome was all-cause mortality (ACM).
Results: The cohort consisted of 360 patients, 259 male/101 female. Median follow-up time was 16 months (IQR: 6.4-42.3); 50 (13.9%) patients experienced CSM, while 218 (61%) experienced ACM. Mean age at surgery was 61 years. Primary clinical tumor size was =7cm in 249/360 (69.2%) of patients. On multivariable Cox regression analysis, primary clinical tumor size =7cm (HR 2.55, p=0.027) and hypertension (HR 3.67, p=0.031) were independently associated with worsened CSM, while papillary type RCC was associated with lowered CSM (HR 0.24, p=0.015). Furthermore primary clinical Tumor size =7cm was associated with an increased risk of ACM (HR 1.47, p=0.026).
Conclusions: Increased primary clinical tumor size =7cm was an independent risk factor associated with worsened CSM and ACM in patients with mRCC. Further investigation is necessary to confirm our findings and to delineate the mechanisms responsible for this phenomenon
Source of Funding: Stephen Weissman Kidney Cancer Research Fund
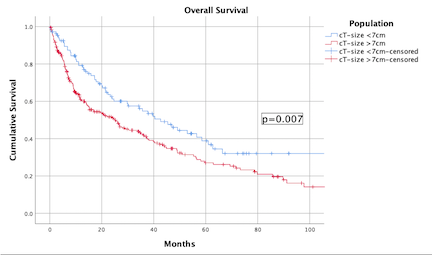
Methods: We performed a multicenter, retrospective analysis using the International Marker Consortium for Renal Cancer (INMARC) identified patients who received CN and systemic therapy from 2001-2019. Demographic and clinical disease factors were analyzed using multivariable Cox regression. KKaplan Meier Analyses (KMA) were conducted to elucidate survival outcomes. Primary outcome was cancer-specific mortality (CSM), secondary outcome was all-cause mortality (ACM).
Results: The cohort consisted of 360 patients, 259 male/101 female. Median follow-up time was 16 months (IQR: 6.4-42.3); 50 (13.9%) patients experienced CSM, while 218 (61%) experienced ACM. Mean age at surgery was 61 years. Primary clinical tumor size was =7cm in 249/360 (69.2%) of patients. On multivariable Cox regression analysis, primary clinical tumor size =7cm (HR 2.55, p=0.027) and hypertension (HR 3.67, p=0.031) were independently associated with worsened CSM, while papillary type RCC was associated with lowered CSM (HR 0.24, p=0.015). Furthermore primary clinical Tumor size =7cm was associated with an increased risk of ACM (HR 1.47, p=0.026).
Conclusions: Increased primary clinical tumor size =7cm was an independent risk factor associated with worsened CSM and ACM in patients with mRCC. Further investigation is necessary to confirm our findings and to delineate the mechanisms responsible for this phenomenon
Source of Funding: Stephen Weissman Kidney Cancer Research Fund

.jpg)
.jpg)