Back
Poster, Podium & Video Sessions
Best Poster Award
MP25: Trauma/Reconstruction/Diversion: Ureter (including Pyeloplasty) and Bladder Reconstruction (including fistula), Augmentation, Substitution, Diversion
MP25-01: Intracorporeal ureterocutaneous urinary diversion after robot-assisted radical cystectomy: outcomes and complications
Saturday, May 14, 2022
10:30 AM – 11:45 AM
Location: Room 228
Serena Tolani*, Etienne Lavallee, John Sfakianos, Reza Mehrazin, Nikhil Waingankar, New York, NY, Sebastian Edeling, Hanover, Germany, Carl Wijburg, Velp, Netherlands, Karel Decaestecker, Ghent, Belgium, Alberto Martini, Francesco Montorsi, Milan, Italy, Abolfazl Hosseini, Peter Wiklund, Stockholm, Sweden
- ST
Poster Presenter(s)
Introduction: Ureterocutaneostomy (UC) urinary diversion is an underutilized procedure due to concern for stoma obstruction from stricture. However, new techniques and procedure revisions have been developed with the aim of improving outcome of UC. Clinical outcomes following intracorporeal UC diversion are currently not well defined in the literature.
Methods: We performed a multicenter retrospective analysis of patients who underwent RARC with intracorporeal UC diversion. The primary endpoint of the study was the risk of ureteral strictures following surgery. Secondary endpoints included peri-operative and oncological outcomes.
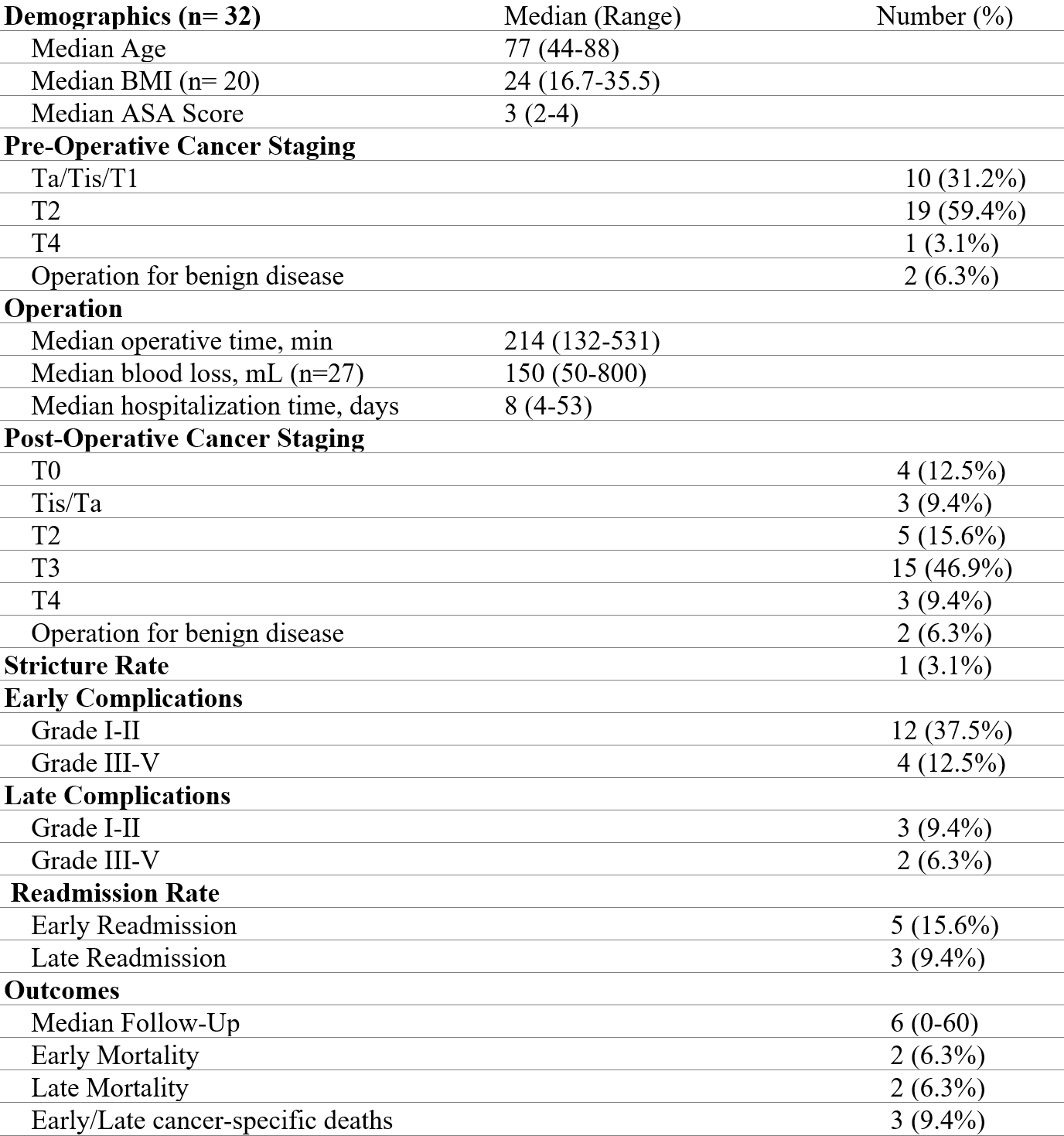
Results: From 2013-2021, 32 patients underwent RARC with UC urinary diversion. 30 patients underwent cystectomy for bladder cancer, while 2 patients had the operation for benign disease. 4 patients had a palliative cystectomy after diagnosis of metastatic bladder cancer. Single J stents were routinely left in place after surgery. The median follow up was 6 months (range 0-60). The median age and ASA score were 77 (range 44-88) and 3 (range 2-4) respectively. The median hospital stay was 8 days (range 4-53). One patient (3.1%) developed a post-operative stricture 5 months after surgery and was treated with stent placement. 56.2% of patients had locally advanced cancer on final pathology (= pT3). Grade III or higher complication occurred in 12.5% of patients within 30 days and in 18.8% of patients within 90 days of surgery. 30-day and 90-day readmission rate were 15.6% and 25% respectively. Four patients died within 90 days of the surgery of whom 2 underwent surgery for palliation. Overall survival was 78%.
Conclusions: To our knowledge, this is the largest cohort of intracorporeal UC urinary diversion. Intracorporeal UC should be considered as an approach to minimize surgical morbidity in patients who may not be candidate for other urinary diversions.
Source of Funding: N/A
Methods: We performed a multicenter retrospective analysis of patients who underwent RARC with intracorporeal UC diversion. The primary endpoint of the study was the risk of ureteral strictures following surgery. Secondary endpoints included peri-operative and oncological outcomes.
Results: From 2013-2021, 32 patients underwent RARC with UC urinary diversion. 30 patients underwent cystectomy for bladder cancer, while 2 patients had the operation for benign disease. 4 patients had a palliative cystectomy after diagnosis of metastatic bladder cancer. Single J stents were routinely left in place after surgery. The median follow up was 6 months (range 0-60). The median age and ASA score were 77 (range 44-88) and 3 (range 2-4) respectively. The median hospital stay was 8 days (range 4-53). One patient (3.1%) developed a post-operative stricture 5 months after surgery and was treated with stent placement. 56.2% of patients had locally advanced cancer on final pathology (= pT3). Grade III or higher complication occurred in 12.5% of patients within 30 days and in 18.8% of patients within 90 days of surgery. 30-day and 90-day readmission rate were 15.6% and 25% respectively. Four patients died within 90 days of the surgery of whom 2 underwent surgery for palliation. Overall survival was 78%.
Conclusions: To our knowledge, this is the largest cohort of intracorporeal UC urinary diversion. Intracorporeal UC should be considered as an approach to minimize surgical morbidity in patients who may not be candidate for other urinary diversions.
Source of Funding: N/A

.jpg)
.jpg)