Back
Poster, Podium & Video Sessions
Moderated Poster
MP25: Trauma/Reconstruction/Diversion: Ureter (including Pyeloplasty) and Bladder Reconstruction (including fistula), Augmentation, Substitution, Diversion
MP25-03: Orthotopic neobladder in female patients with bladder cancer: long-term functional outcomes and the role of surgical technique
Saturday, May 14, 2022
10:30 AM – 11:45 AM
Location: Room 228
Seyedeh Sanam Ladi Seyedian*, Mitchell Goldenburg, Muhannad Alsyouf, Sumeet Bhanvadia, Hooman Djaladat, Anne Schuckman, David Ginsberg, Siamak Daneshmand, Los Angeles, CA
Seyedeh Sanam Ladi Seyedian, MD
University of Southern California
Poster Presenter(s)
Introduction: Although orthotopic diversion with ileal neobladder is a well-established option for women undergoing radical cystectomy, functional outcomes are heterogenous and often hard to predict. Importantly, these outcomes have not been compared across female organ-sparing approaches. We aim to compare functional outcomes of patients undergoing anterior pelvic exenteration (APE), vaginal-sparing cystectomy (VSC), and female organ-sparing cystectomy (FOSC) and assess predictors of post-operative continence and retention.
Methods: Using our institutional review board approved bladder cancer database, we identified 73 female patients who underwent open radical cystectomy and orthotopic neobladder from 2010 to 2020. Patients with a minimum follow of 6 months were included in final analysis. Clinicopathologic information, including daily pad number, degree of wetness and catheter use were abstracted. Urinary retention was defined as =3 catheterisations/day or a self-reported inability to void without a catheter. Patients were considered continent if they reported no pad use or pads “almost dry” during a given time (day or night).
Results: A total of 57 female patients with adequate follow up were included. The median age was 65 years (IQR: 59-71). Of these, 32 (56%) had APE, 16 (28%) had VSC, and 9 (16%) had FOSC. Urinary retention was seen in 19/57 (33%) of patients, of whom 12/19 (63%) and 6/19 (31.5%) underwent APE and VSC, respectively, with a median time to retention of 12 months (IQR 7 -16.7).
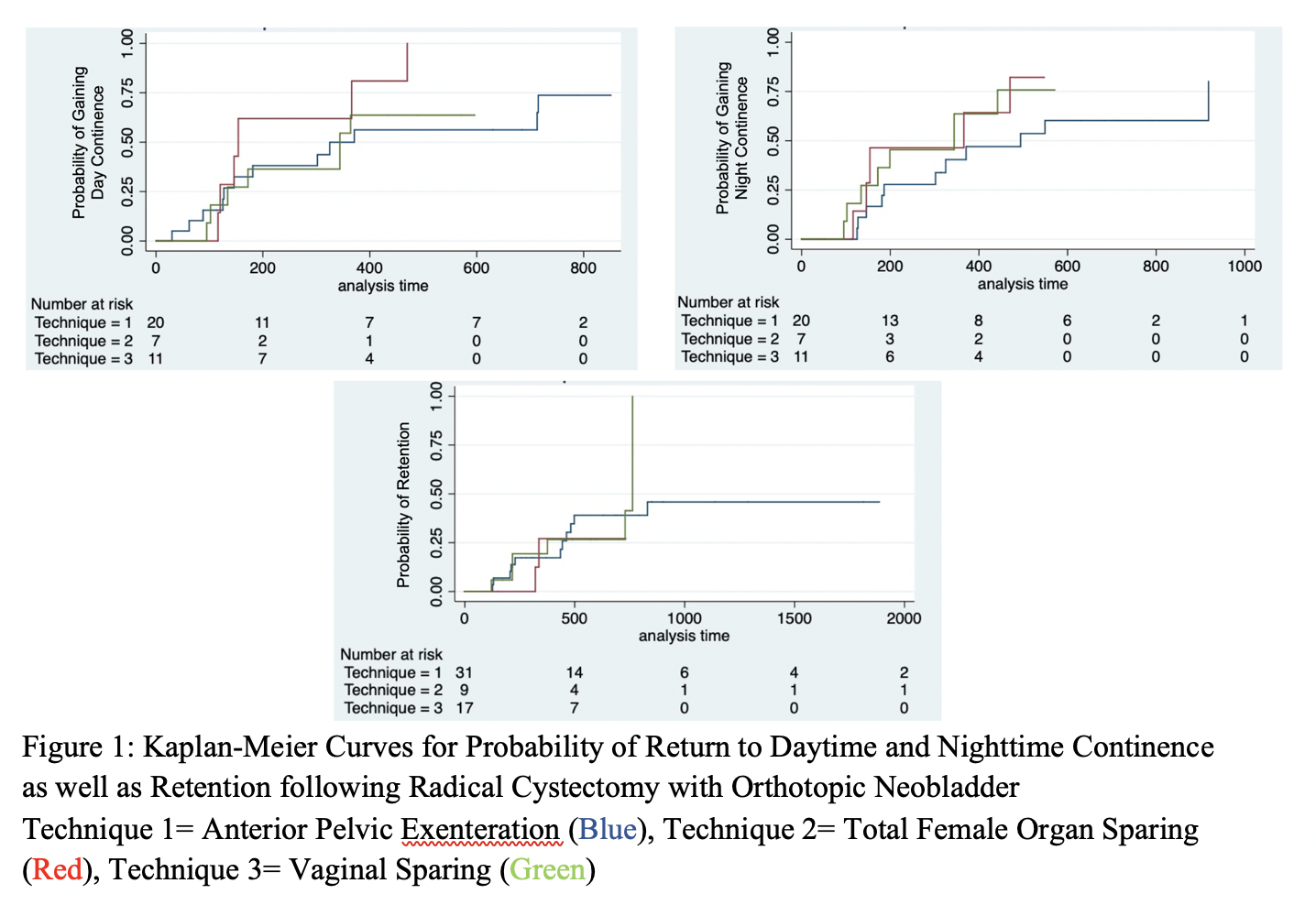
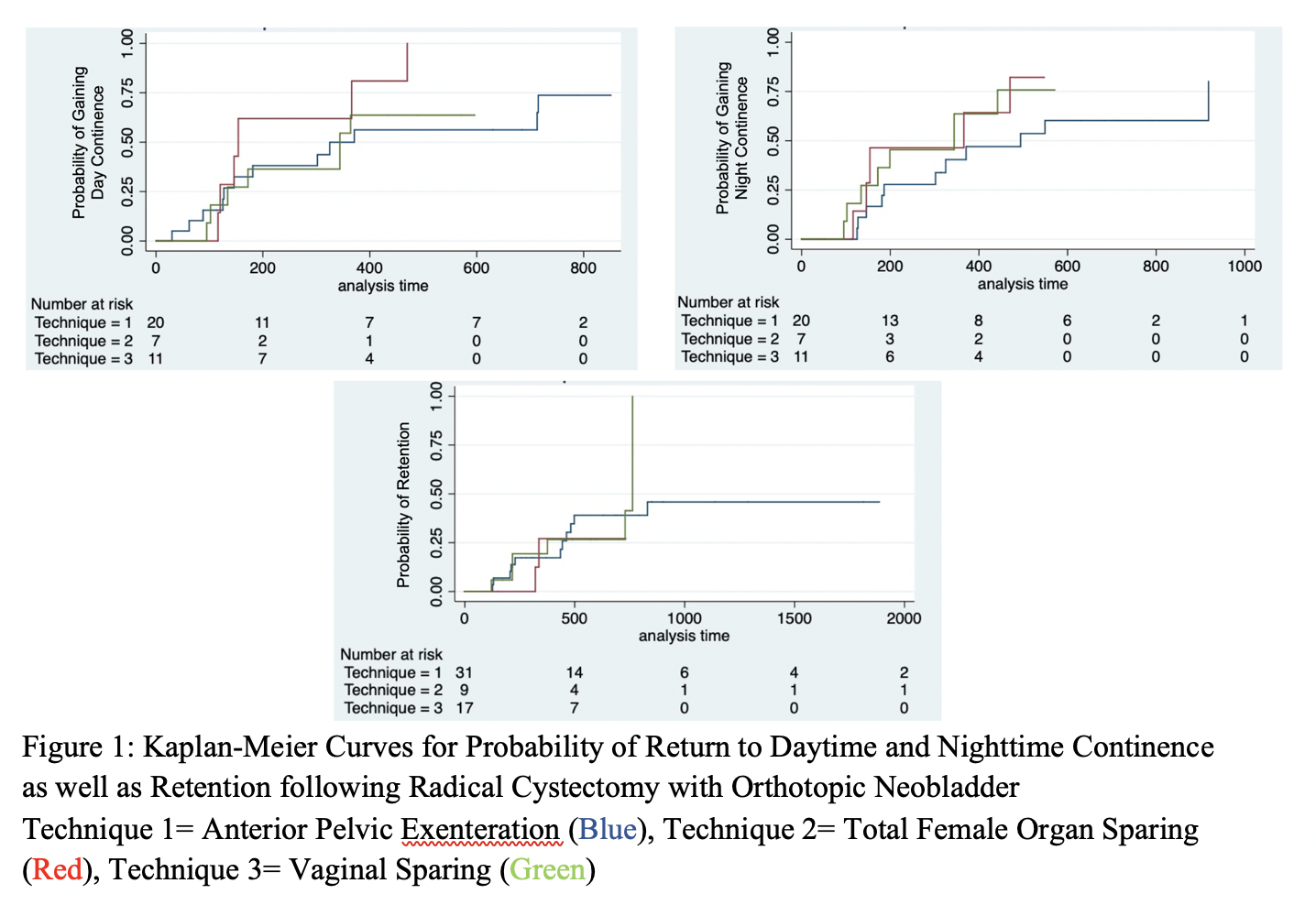
Among patients not in retention (38/57, 66%), day and nighttime continence rates at 24 months post-operatively were 85% and 65% respectively. At one year following surgery, 85% of FOSC patients recovered daytime continence compared to 65% in APE and 64% in VSC (figure 1).
On univariate cox regression, history of vaginal delivery (HR 5, P=0.005) was associated with daytime incontinence. Peri-operative chemotherapy (HR 4, P=0.02), nodal involvement (HR 13, P=0.02) and pathological stage >T3 (HR 5, P=0.002) were risk factors for retention.
Conclusions: Our data suggests that female organ-sparing techniques may offer improved functional outcomes in women undergoing neobladder creation at cystectomy. Day and night continence appear to improve over time, regardless of the surgical technique.
Source of Funding: None
Methods: Using our institutional review board approved bladder cancer database, we identified 73 female patients who underwent open radical cystectomy and orthotopic neobladder from 2010 to 2020. Patients with a minimum follow of 6 months were included in final analysis. Clinicopathologic information, including daily pad number, degree of wetness and catheter use were abstracted. Urinary retention was defined as =3 catheterisations/day or a self-reported inability to void without a catheter. Patients were considered continent if they reported no pad use or pads “almost dry” during a given time (day or night).
Results: A total of 57 female patients with adequate follow up were included. The median age was 65 years (IQR: 59-71). Of these, 32 (56%) had APE, 16 (28%) had VSC, and 9 (16%) had FOSC. Urinary retention was seen in 19/57 (33%) of patients, of whom 12/19 (63%) and 6/19 (31.5%) underwent APE and VSC, respectively, with a median time to retention of 12 months (IQR 7 -16.7).
Among patients not in retention (38/57, 66%), day and nighttime continence rates at 24 months post-operatively were 85% and 65% respectively. At one year following surgery, 85% of FOSC patients recovered daytime continence compared to 65% in APE and 64% in VSC (figure 1).
On univariate cox regression, history of vaginal delivery (HR 5, P=0.005) was associated with daytime incontinence. Peri-operative chemotherapy (HR 4, P=0.02), nodal involvement (HR 13, P=0.02) and pathological stage >T3 (HR 5, P=0.002) were risk factors for retention.
Conclusions: Our data suggests that female organ-sparing techniques may offer improved functional outcomes in women undergoing neobladder creation at cystectomy. Day and night continence appear to improve over time, regardless of the surgical technique.
Source of Funding: None

.jpg)
.jpg)