Back
Poster, Podium & Video Sessions
Moderated Poster
MP26: Stone Disease: Epidemiology & Evaluation I
MP26-02: Prevalence of 24-Hour Urine Abnormalities among Older Adults with Urinary Stone Disease
Saturday, May 14, 2022
10:30 AM – 11:45 AM
Location: Room 225
Ryan Hsi*, Nashville, TN, Mary Oerline, Ann Arbor, MI, Joseph Crivelli, Birmingham, AL, Vahakn Shahinian, John Hollingsworth, Ann Arbor, MI

Ryan S. Hsi, MD,FACS
Vanderbilt University Medical Center
Poster Presenter(s)
Introduction: While urinary stone disease (USD) is traditionally considered a condition affecting working age adults, its prevalence among the older population is increasing. Given physiologic and lifestyle differences between these two populations, there is reason to believe that the frequency of urine chemistry abnormalities may also differ in older adults. In this context, we characterized 24-hour urine findings in a large convenience sample of Medicare beneficiaries.
Methods: For our study, we analyzed urine chemistry data from Medicare beneficiaries 65 years of age and older with a diagnosis of USD, who had a 24-hour urine specimen processed by a large central laboratory in the U.S. between 2010 to 2019. For beneficiaries with multiple submitted specimens, we extracted analyte values from their first collection. Using laboratory reference ranges, we then determined whether a given beneficiary had evidence of hypercalciuria, hyperoxaluria, hypocitraturia, hyperuricosuria, or abnormal urine pH. Finally, we examined the frequency of multiple abnormalities (2, 3, and 4 or more) on a single collection.
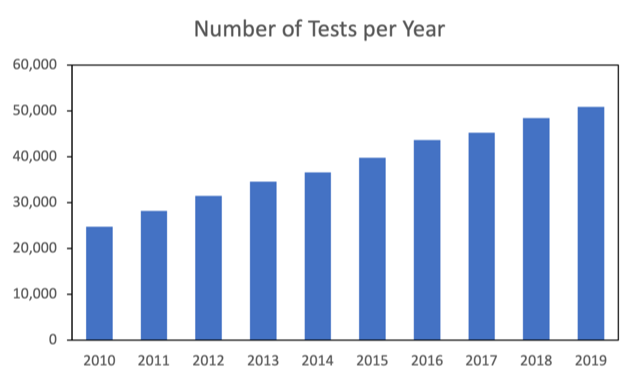
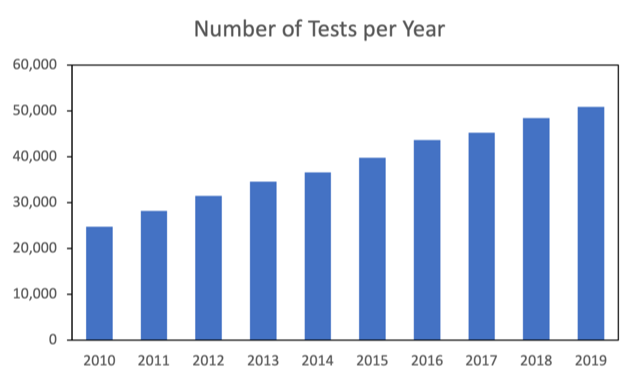
Results: A total of 196,297 beneficiaries underwent 24-hour urine testing for USD. The tests increased from 24,744 in 2010 to 50,936 in 2019 (Figure 1). The sample adequacy, as determined by urine creatinine per body weight, was normally distributed (mean ± SD, 15.0 ± 4.5 mg/kg). Low urine volume was the most common abnormality (urine output less than 2 L/day in 61.9%), followed by hypocitraturia (43.8%), hyperoxaluria (34.2%), hypercalciuria (25%), and hyperuricosuria (17.3%). Twenty-five percent and 31.4% of beneficiaries had high and low urine pH, respectively. High urine sodium was observed in 17.3%. The percentages of beneficiaries with 2, 3, and 4 or more concurrent abnormalities were 33.9%, 35.2%, and 15.8%, respectively.
Conclusions: Older adults with USD frequently have urine chemistry abnormalities, and often more than one abnormality is present. These data suggest that 24-hour urine testing in this population can help providers select interventions to help reduce future stone risk.
Source of Funding: NIDDK R01DK121709
Methods: For our study, we analyzed urine chemistry data from Medicare beneficiaries 65 years of age and older with a diagnosis of USD, who had a 24-hour urine specimen processed by a large central laboratory in the U.S. between 2010 to 2019. For beneficiaries with multiple submitted specimens, we extracted analyte values from their first collection. Using laboratory reference ranges, we then determined whether a given beneficiary had evidence of hypercalciuria, hyperoxaluria, hypocitraturia, hyperuricosuria, or abnormal urine pH. Finally, we examined the frequency of multiple abnormalities (2, 3, and 4 or more) on a single collection.
Results: A total of 196,297 beneficiaries underwent 24-hour urine testing for USD. The tests increased from 24,744 in 2010 to 50,936 in 2019 (Figure 1). The sample adequacy, as determined by urine creatinine per body weight, was normally distributed (mean ± SD, 15.0 ± 4.5 mg/kg). Low urine volume was the most common abnormality (urine output less than 2 L/day in 61.9%), followed by hypocitraturia (43.8%), hyperoxaluria (34.2%), hypercalciuria (25%), and hyperuricosuria (17.3%). Twenty-five percent and 31.4% of beneficiaries had high and low urine pH, respectively. High urine sodium was observed in 17.3%. The percentages of beneficiaries with 2, 3, and 4 or more concurrent abnormalities were 33.9%, 35.2%, and 15.8%, respectively.
Conclusions: Older adults with USD frequently have urine chemistry abnormalities, and often more than one abnormality is present. These data suggest that 24-hour urine testing in this population can help providers select interventions to help reduce future stone risk.
Source of Funding: NIDDK R01DK121709

.jpg)
.jpg)