Back
Poster, Podium & Video Sessions
Moderated Poster
MP26: Stone Disease: Epidemiology & Evaluation I
MP26-14: Associations of Food Access and Neighborhood Walkability with Urinary Risk Factors for Kidney Stone Disease
Saturday, May 14, 2022
10:30 AM – 11:45 AM
Location: Room 225
Joseph Crivelli*, David Redden, Birmingham, AL, Naim Maalouf, Dallas, TX, Kyle Wood, Dean Assimos, Gabriela Oates, Birmingham, AL

Joseph J. Crivelli, MD
University of Alabama at Birmingham School of Medicine
Poster Presenter(s)
Introduction: Differences in nutrition and lifestyle can explain some differences in 24-hour urine measurements among kidney stone formers. Socioeconomic aspects of these factors underlying stone formation require further investigation. We evaluated associations of neighborhood indices of food access and walkability with 24-hour urine measurements among patients with kidney stone disease (KSD).
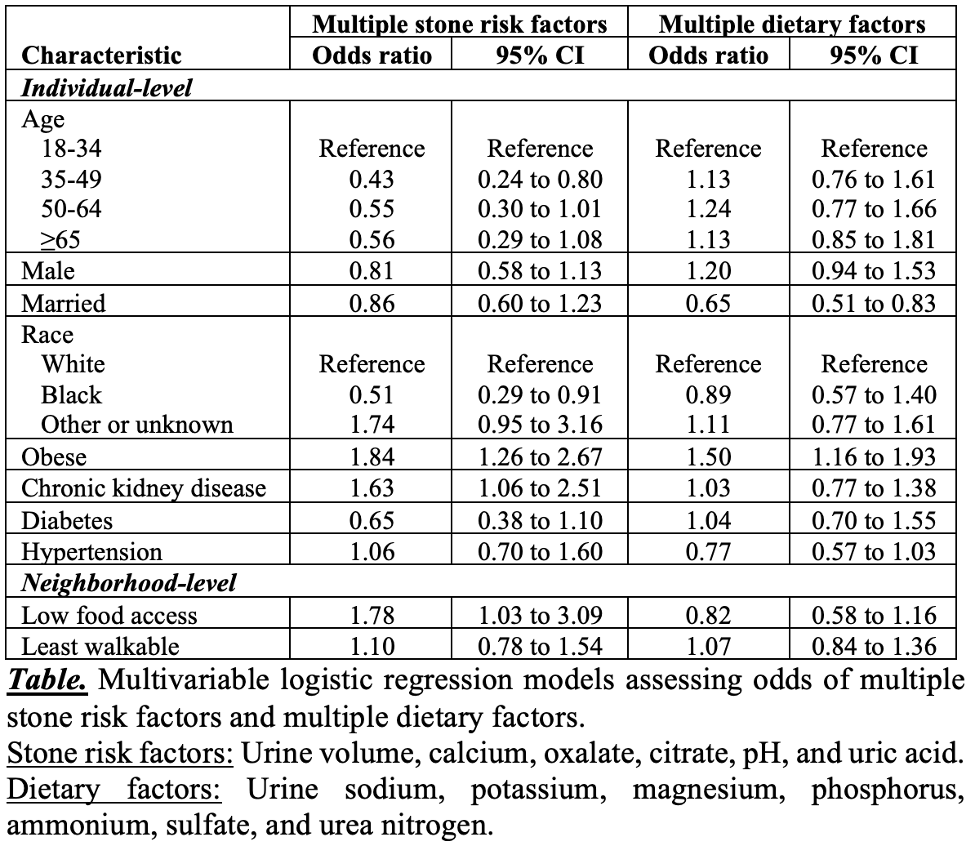
Methods: We performed a retrospective analysis of adult patients with KSD evaluated with 24-hour urine collection (2001-2020). Based on the Food Access Research Atlas, low-income neighborhoods >0.5 miles (urban areas) or >10 miles (rural areas) from a full-service grocery store met the definition of low food access. Using the National Walkability Index (NWI), we identified neighborhoods with low walkability (NWI =5.75). We then assessed associations of these measures of food access and walkability with groupings of 24-hour urine abnormalities (stone risk factors and dietary factors, as defined by a commercial vendor; see Table) through multivariable logistic regression, as well as individual 24-hour urine measurements through analysis of covariance (ANCOVA) with adjustment for multiple testing.
Results: Among 1,119 patients with KSD and at least one adequate 24-hour urine collection based on urinary creatinine, 173 (15.5%) were from neighborhoods with low food access and 516 (46.1%) were from neighborhoods with low walkability. Using multivariable logistic regression (Table), patients from neighborhoods with low food access had higher odds of multiple (>1) stone risk factors (odds ratio: 1.78, 95% confidence interval: 1.03 to 3.09), but not multiple dietary factors. Patients from neighborhoods with low walkability did not have increased odds of multiple stone risk factors or dietary factors. Using ANCOVA, neighborhoods with low food access and or low walkability were not associated with significant differences in individual 24-hour urine measurements.
Conclusions: Among patients with KSD, residence in a neighborhood with low food access was associated with multiple stone risk factors on 24-hour urine testing, though there were no significant differences in individual urinary measurements. The contribution of other sociodemographic factors to 24-hour urine abnormalities should be evaluated.
Source of Funding: NIH 5P20DK119788 (DA) and 5K08DK115833 (KW)
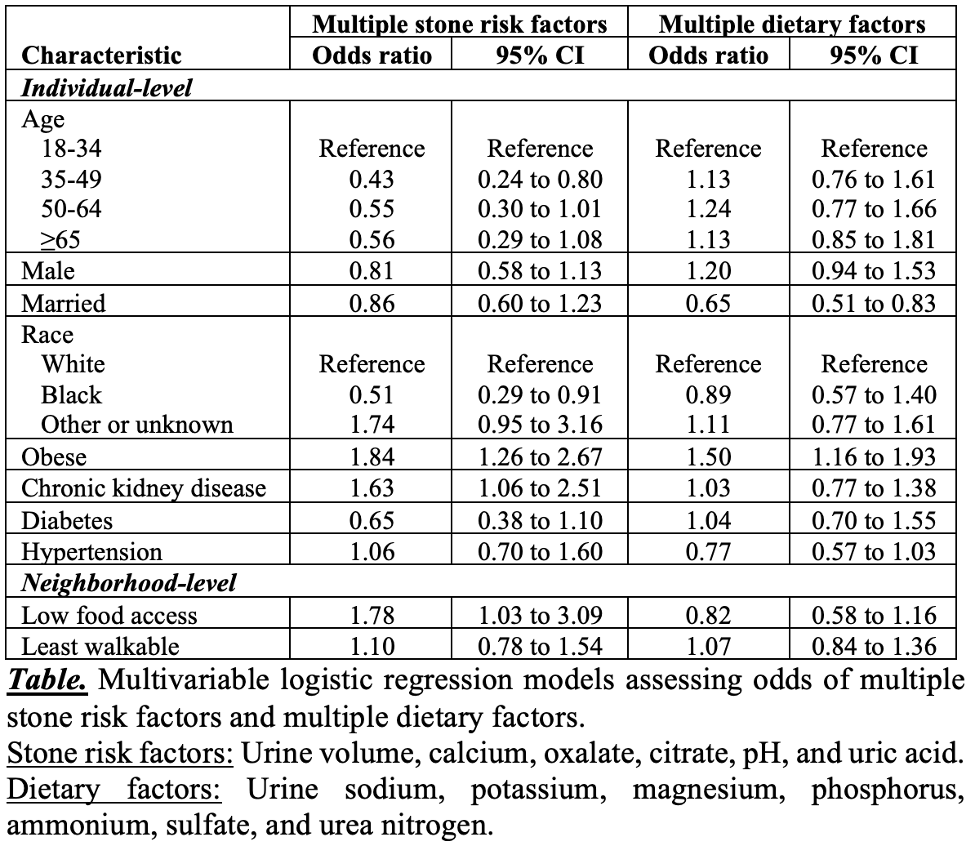
Methods: We performed a retrospective analysis of adult patients with KSD evaluated with 24-hour urine collection (2001-2020). Based on the Food Access Research Atlas, low-income neighborhoods >0.5 miles (urban areas) or >10 miles (rural areas) from a full-service grocery store met the definition of low food access. Using the National Walkability Index (NWI), we identified neighborhoods with low walkability (NWI =5.75). We then assessed associations of these measures of food access and walkability with groupings of 24-hour urine abnormalities (stone risk factors and dietary factors, as defined by a commercial vendor; see Table) through multivariable logistic regression, as well as individual 24-hour urine measurements through analysis of covariance (ANCOVA) with adjustment for multiple testing.
Results: Among 1,119 patients with KSD and at least one adequate 24-hour urine collection based on urinary creatinine, 173 (15.5%) were from neighborhoods with low food access and 516 (46.1%) were from neighborhoods with low walkability. Using multivariable logistic regression (Table), patients from neighborhoods with low food access had higher odds of multiple (>1) stone risk factors (odds ratio: 1.78, 95% confidence interval: 1.03 to 3.09), but not multiple dietary factors. Patients from neighborhoods with low walkability did not have increased odds of multiple stone risk factors or dietary factors. Using ANCOVA, neighborhoods with low food access and or low walkability were not associated with significant differences in individual 24-hour urine measurements.
Conclusions: Among patients with KSD, residence in a neighborhood with low food access was associated with multiple stone risk factors on 24-hour urine testing, though there were no significant differences in individual urinary measurements. The contribution of other sociodemographic factors to 24-hour urine abnormalities should be evaluated.
Source of Funding: NIH 5P20DK119788 (DA) and 5K08DK115833 (KW)

.jpg)
.jpg)