Back
Poster, Podium & Video Sessions
Moderated Poster
MP27: Prostate Cancer: Advanced (including Drug Therapy) I
MP27-04: Oncologic Outcomes in Men with Adverse Pathology and Biochemical Persistence After Radical Prostatectomy
Saturday, May 14, 2022
10:30 AM – 11:45 AM
Location: Room 222
Marlon Perera, Amy Tin, Benjamin Beech*, Daniel Sjoberg, Nicole Benfante, Jaspreet Sandhu, Vincent Laudone, Behfar Ehdaie, James Eastham, Peter Scardino, Karim Touijer, New York, NY

Benjamin Beech, MD, FRCSC
Memorial Sloan Kettering Cancer Center
Poster Presenter(s)
Introduction: Pathologic nodal invasion in patients post-prostatectomy is becoming increasingly pertinent, particularly in light of the recent trend towards operative intervention in patients harboring high risk disease. PSA persistence post-operatively poses a management dilemma, with a stark absence of recommendations by authoritative guidelines. We aimed to highlight the experience of this clinical scenario at a high volume institution and report long-term oncologic outcomes.
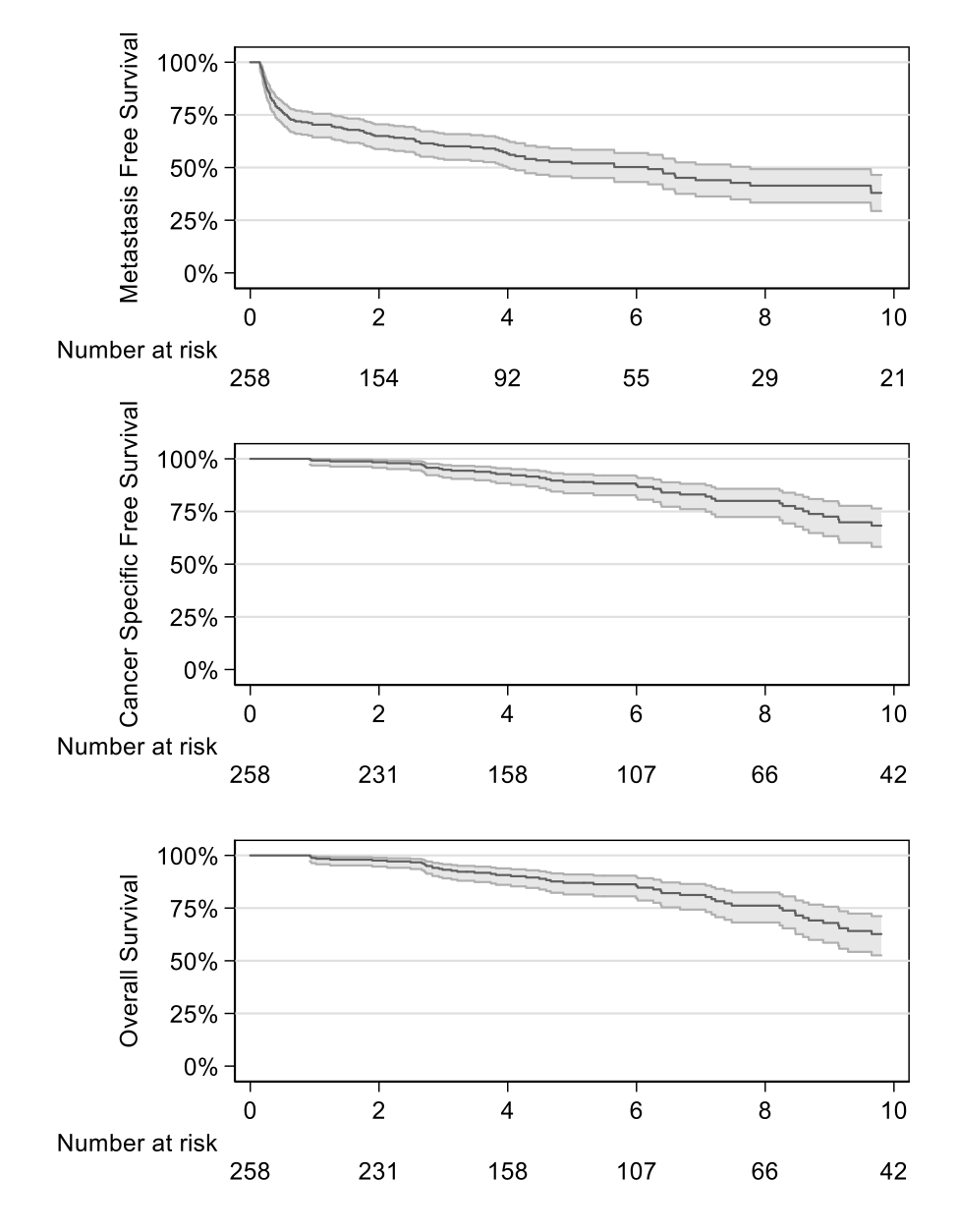
Methods: We identified patients who underwent radical prostatectomy between 1988 and 2017, had lymph node involvement, and had persistent elevated prostate-specific antigen. Post-operative imaging and management strategies were collated. Probability of metastasis-free survival (MFS), prostate cancer specific survival (CSS) and overall survival (OS) among this cohort of men using Kaplan-Meier methods.
Results: We identified 258 patients meeting the elgibility criteria, of which 128 patients developed metastasis. The 5-year and 10-year MFS probability was 52% (95% CI 45%, 58%) and 38% (95% CI 29%, 47%), respectively. We identified 58 patients who died of any cause, 48 from disease. The 5 and 10-year survival probabilities from disease are 89% (95% CI 84%, 93%), and 68% (95% CI 58%, 76%), respectively; and from any cause are 87% (95% CI 81%, 91%), and 63% (95% CI 53%, 71%), respectively. Post-operative imaging was obtained for 77% of patients, of whom 87% had a negative scan. Post-operative treatment included hormonal deprivation in 88% of men, observation alone in 7%, adjuvant radiotherapy in 4%, and combined chemotherapy and hormonal therapy in 1%.
Conclusions: In the absence of clear pre-existing data or guidelines, we highlight our experience of patients with nodal invasion and PSA persistence post-prostatectomy. We highlight compromised metastatases-free survival and overall survival. Further, we highlight the limited role for conventional imaging in this cohort.
Source of Funding: Sidney Kimmel Center for Prostate and Urologic Cancers at MSKCC and NIH/NCI grants P50CA092629. Marlon Perera is sponsored by the Australian-America Fulbright Commission administered through a 2021-2022 Fulbright Future Scholarship funded by The Kinghorn Foundation.
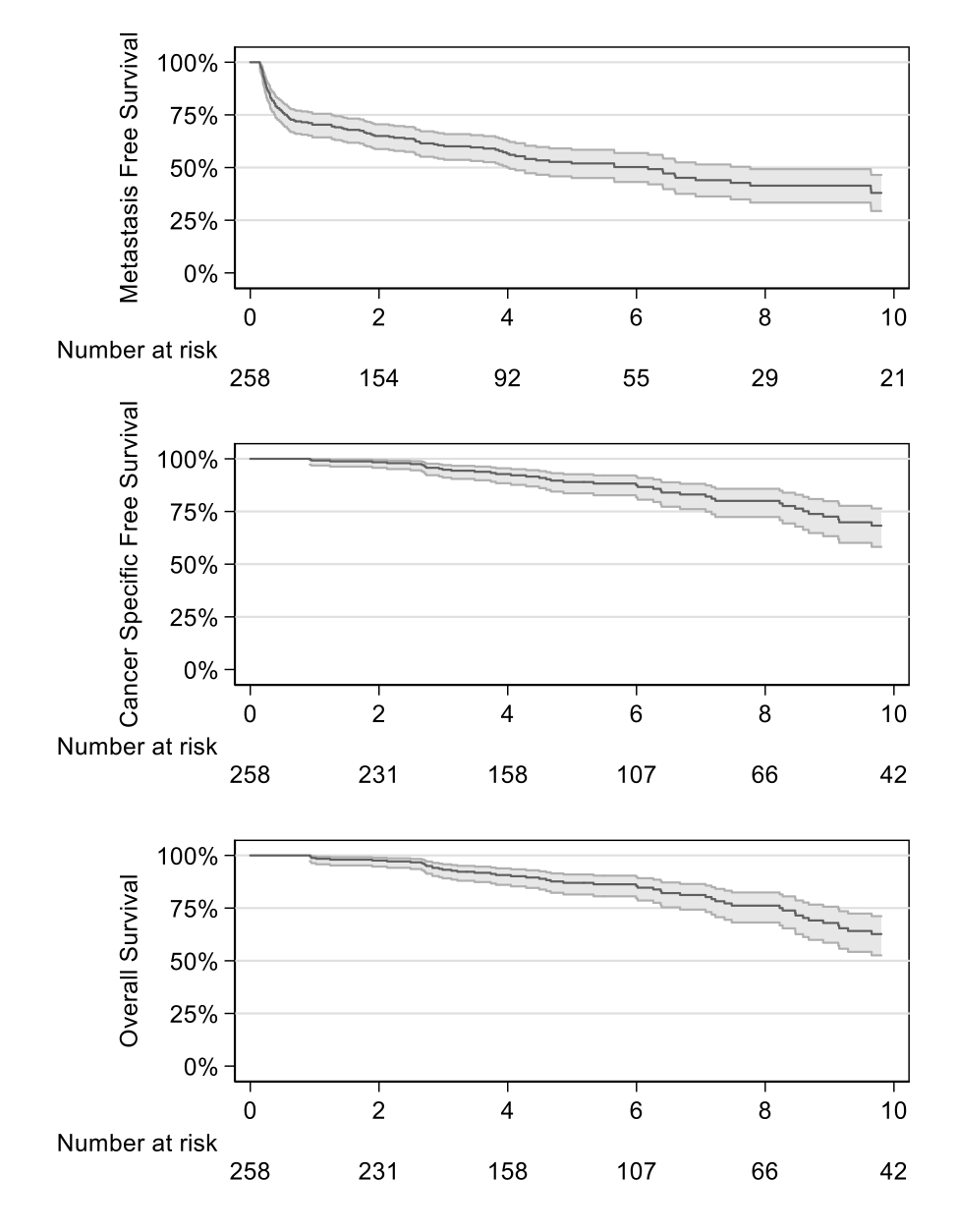
Methods: We identified patients who underwent radical prostatectomy between 1988 and 2017, had lymph node involvement, and had persistent elevated prostate-specific antigen. Post-operative imaging and management strategies were collated. Probability of metastasis-free survival (MFS), prostate cancer specific survival (CSS) and overall survival (OS) among this cohort of men using Kaplan-Meier methods.
Results: We identified 258 patients meeting the elgibility criteria, of which 128 patients developed metastasis. The 5-year and 10-year MFS probability was 52% (95% CI 45%, 58%) and 38% (95% CI 29%, 47%), respectively. We identified 58 patients who died of any cause, 48 from disease. The 5 and 10-year survival probabilities from disease are 89% (95% CI 84%, 93%), and 68% (95% CI 58%, 76%), respectively; and from any cause are 87% (95% CI 81%, 91%), and 63% (95% CI 53%, 71%), respectively. Post-operative imaging was obtained for 77% of patients, of whom 87% had a negative scan. Post-operative treatment included hormonal deprivation in 88% of men, observation alone in 7%, adjuvant radiotherapy in 4%, and combined chemotherapy and hormonal therapy in 1%.
Conclusions: In the absence of clear pre-existing data or guidelines, we highlight our experience of patients with nodal invasion and PSA persistence post-prostatectomy. We highlight compromised metastatases-free survival and overall survival. Further, we highlight the limited role for conventional imaging in this cohort.
Source of Funding: Sidney Kimmel Center for Prostate and Urologic Cancers at MSKCC and NIH/NCI grants P50CA092629. Marlon Perera is sponsored by the Australian-America Fulbright Commission administered through a 2021-2022 Fulbright Future Scholarship funded by The Kinghorn Foundation.

.jpg)
.jpg)