Back
Poster, Podium & Video Sessions
Moderated Poster
MP27: Prostate Cancer: Advanced (including Drug Therapy) I
MP27-19: Comparative out-of-pocket costs of treatment options in privately insured patients with advanced prostate cancer
Saturday, May 14, 2022
10:30 AM – 11:45 AM
Location: Room 222
Daniel D. Joyce*, Vidit Sharma, David H. Jiang, Holly K. Van Houten, Lindsey R. Sangaralingham, Eugene D. Kwon, Rochester, MN, David F. Penson, Stacie B. Dusetzina, Nashville, TN, Jon C. Tilburt, Scottsdale, AZ, Stephen A. Boorjian, Rochester, MN

Daniel Joyce, MD
Mayo Clinic, Rochester, MN
Poster Presenter(s)
Introduction: The out-of-pocket costs (OOPC) associated with treatment options for advanced prostate cancer are understudied. We describe and identify patient level predictors of OOPC associated with advanced prostate cancer treatments.
Methods: Using the OptumLabs claims dataset, we identified all privately insured men with available OOPC receiving systemic therapy for advanced prostate cancer (biochemical recurrent or metastatic) from 2007-2019. Patients were divided into three treatment groups: androgen deprivation (ADT) monotherapy (i.e. leuprolide/degarelix); novel hormonal (abiraterone, enzalutamide, apalutamide, darolutamide); non-hormonal (chemotherapy, immunotherapy). The primary outcome was OOPC in the first year of treatment. Group allocation and patient factors were associated with OOPC using multivariable regressions with generalized linear models with gamma distributions. All costs were adjusted to reflect 2019 U.S. dollars using the consumer price index.
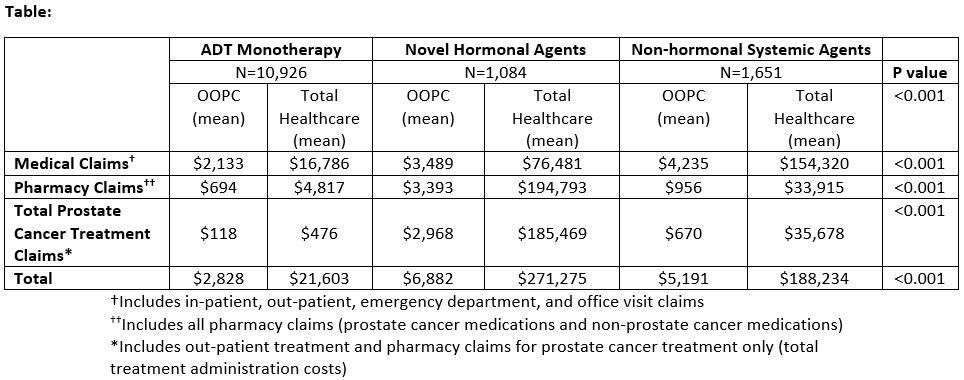
Results: In a cohort of 13,661 men, there were 80% (n=10,926) receiving ADT monotherapy, 8% (n=1,084) receiving novel hormonal treatments, and 12% (n=1,651) receiving non-hormonal treatments. Mean OOPC in the first year of treatment were $2,828, $6,882, and $5,191 for ADT monotherapy, novel hormonal, and non-hormonal treatments, respectively (Table). On multivariable analysis, novel hormonal (coeff: 1.99, p<0.001) and non-hormonal (coeff: 1.70, p<0.001) treatments were associated with increased total OOPC in the first year of treatment compared to ADT monotherapy. Patient factors associated (p < 0.001) with higher OOPC included: older age, Asian/Hispanic race/ethnicity, and comorbidity.
Conclusions: Patients receiving novel hormonal agents had substantially higher OOPC than other therapies. In addition to raising awareness among prescribers, these data support the inclusion of financial toxicity discussions as a part of patient counseling for these agents.
Source of Funding: None
Methods: Using the OptumLabs claims dataset, we identified all privately insured men with available OOPC receiving systemic therapy for advanced prostate cancer (biochemical recurrent or metastatic) from 2007-2019. Patients were divided into three treatment groups: androgen deprivation (ADT) monotherapy (i.e. leuprolide/degarelix); novel hormonal (abiraterone, enzalutamide, apalutamide, darolutamide); non-hormonal (chemotherapy, immunotherapy). The primary outcome was OOPC in the first year of treatment. Group allocation and patient factors were associated with OOPC using multivariable regressions with generalized linear models with gamma distributions. All costs were adjusted to reflect 2019 U.S. dollars using the consumer price index.
Results: In a cohort of 13,661 men, there were 80% (n=10,926) receiving ADT monotherapy, 8% (n=1,084) receiving novel hormonal treatments, and 12% (n=1,651) receiving non-hormonal treatments. Mean OOPC in the first year of treatment were $2,828, $6,882, and $5,191 for ADT monotherapy, novel hormonal, and non-hormonal treatments, respectively (Table). On multivariable analysis, novel hormonal (coeff: 1.99, p<0.001) and non-hormonal (coeff: 1.70, p<0.001) treatments were associated with increased total OOPC in the first year of treatment compared to ADT monotherapy. Patient factors associated (p < 0.001) with higher OOPC included: older age, Asian/Hispanic race/ethnicity, and comorbidity.
Conclusions: Patients receiving novel hormonal agents had substantially higher OOPC than other therapies. In addition to raising awareness among prescribers, these data support the inclusion of financial toxicity discussions as a part of patient counseling for these agents.
Source of Funding: None

.jpg)
.jpg)