Back
Poster, Podium & Video Sessions
Moderated Poster
MP28: Health Services Research: Practice Patterns, Quality of Life and Shared Decision Making III
MP28-04: Validation of a surgical decision aid for patients with nephrolithiasis: Shockwave lithotripsy versus ureteroscopy
Saturday, May 14, 2022
1:00 PM – 2:15 PM
Location: Room 228
John Michael DiBianco*, Stephanie Daignault-Newton, Bronson Conrado, Sarah T. Hawley, Giulia Lane, Khurshid R. Ghani, Casey A. Dauw, for the Michigan Urological Surgery Improvement Collaborative, Ann Arbor, MI
.jpg)
John M. Dibianco, MD
University of Michigan
Poster Presenter(s)
Introduction: Shared decision making is recommended for patients with symptomatic nephrolithiasis to assist the deciding between ureteroscopy (URS) or shockwave lithotripsy (SWL). The practice of shared decision making remains low in this population. We aimed to develop a surgical decision aid (SDA) to facilitate treatment decision making for patients with nephrolithiasis.
Methods: The scope of the SDA was identified through discussions with patients, patient advocates and urologists in the Michigan Urological Surgery Improvement Collaborative (MUSIC). A steering committee consisted of patient advocates, MUSIC coordinating center, decision making content experts, biostatisticians and MUSIC urologists. Content domains were assessed through best available evidence and expert opinion. For content validation we conducted anonymous survey of 35 MUSIC urologists. Content Validity Ratios (CVR), numeric value indicating degree of expert validity, were calculated. Face validation interviews were conducted with patient advocates.
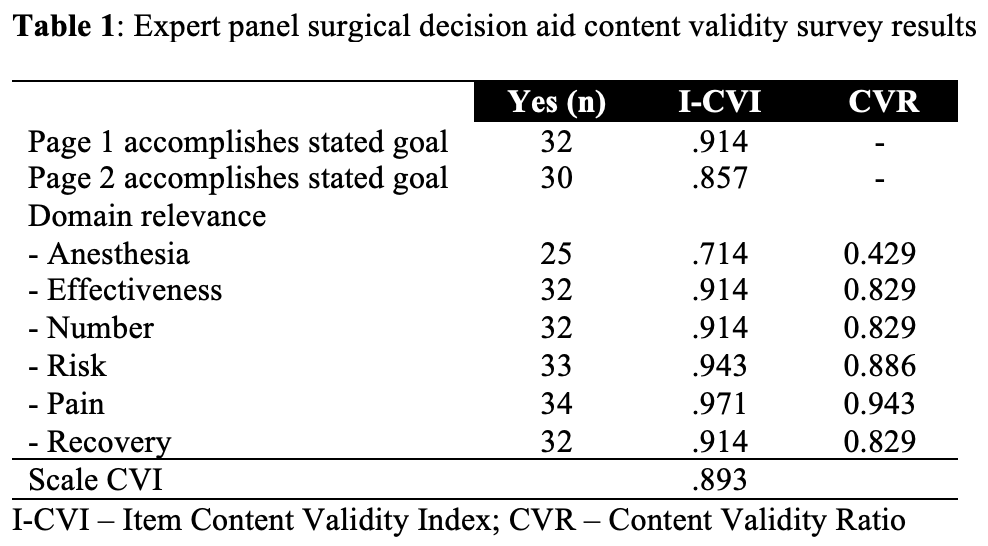
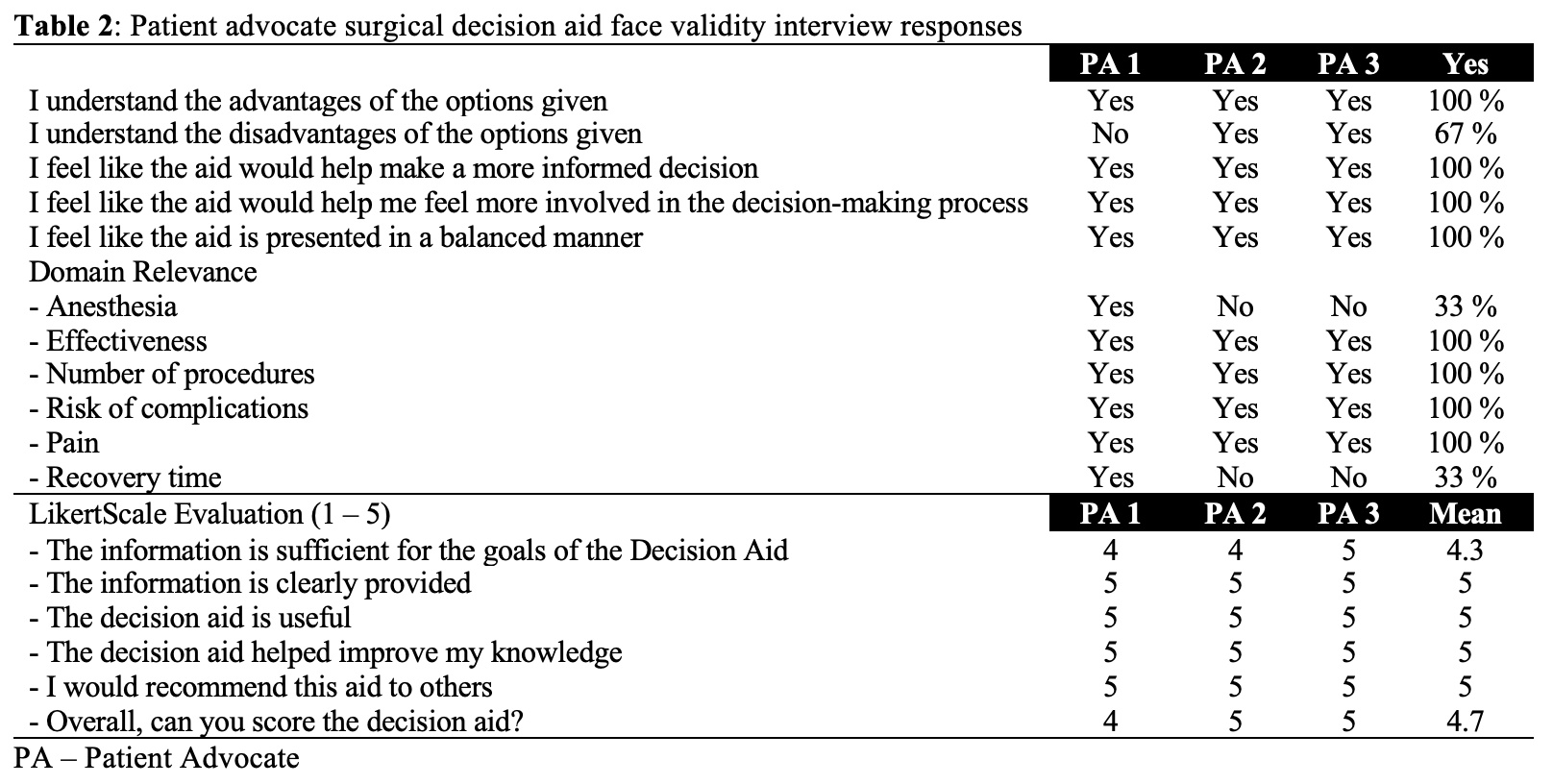
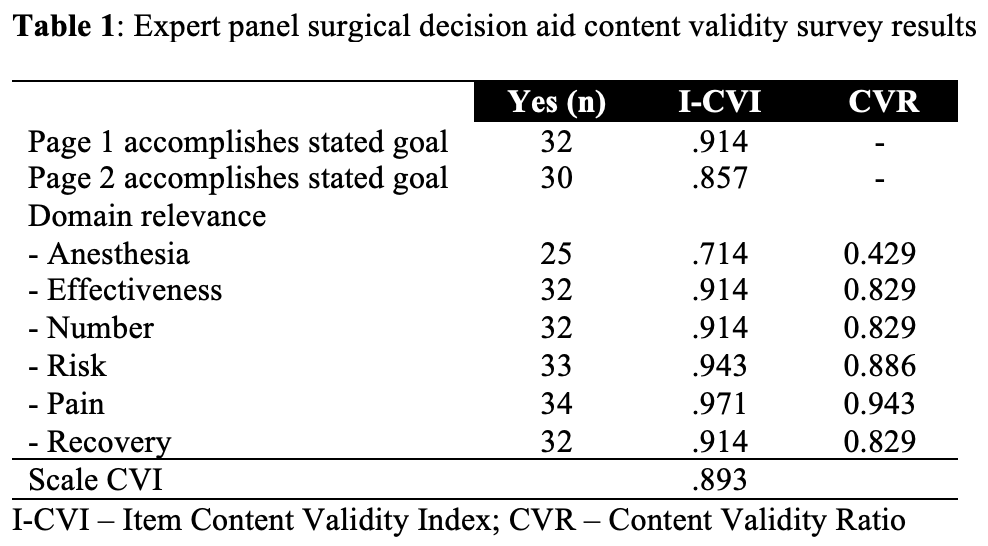
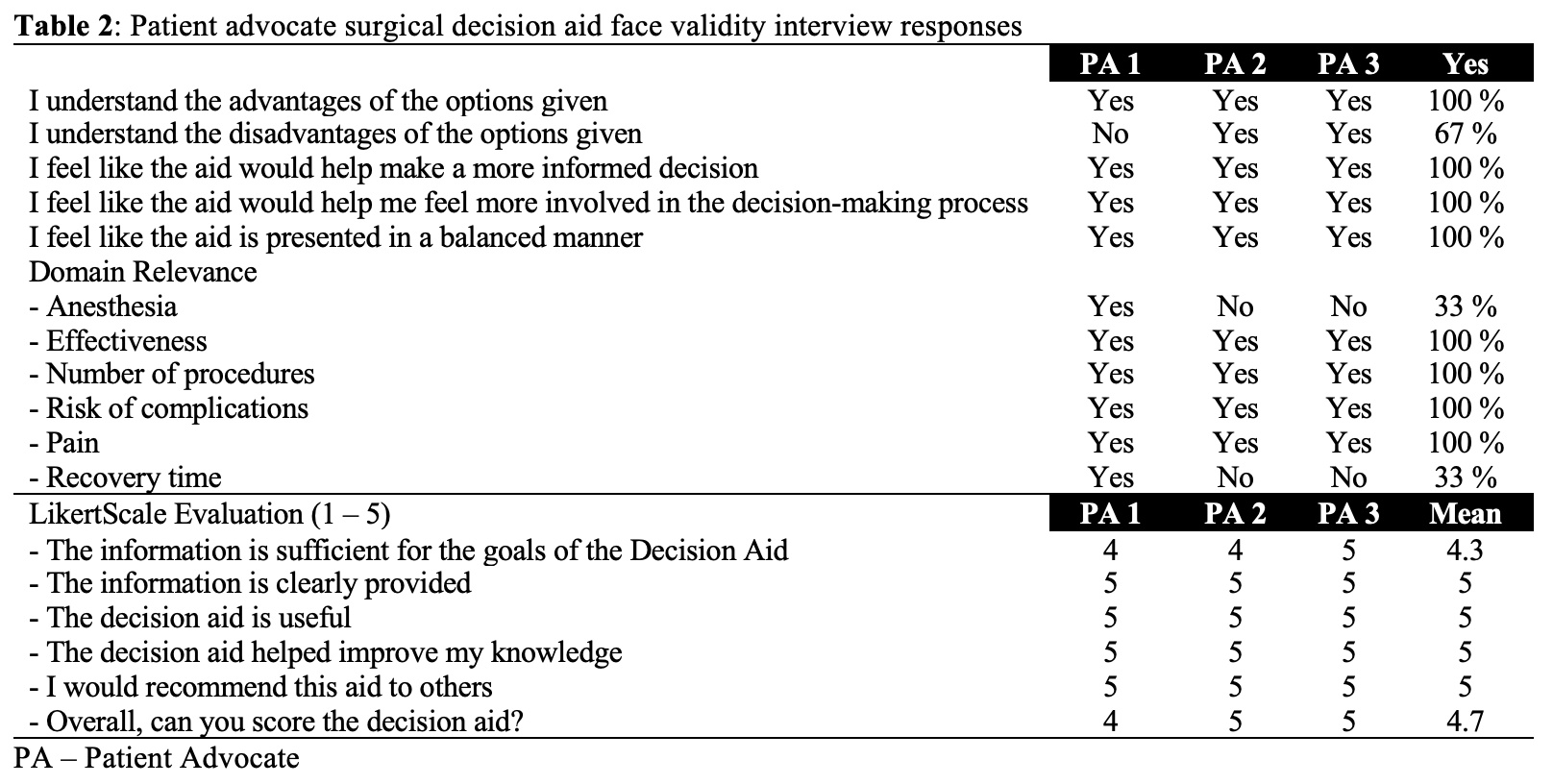
Results: A prototype using descriptive plain language and pictorial information was designed for nephrolithiasis patients who are candidates for SWL or URS. Page 1 addressed patient education and page 2 informed urologists of patient treatment goals. Six content domains were chosen: anesthesia type, effectiveness, number of procedures, risk, pain and recovery. 91.4% and 85.7% of urologists indicated that Page 1 and Page 2 accomplished their goals, respectively (Table 1). Anesthesia type was the only domain to receive a lower than acceptable CVR. Patient advocates reported high levels of face validation (Table 2).
Conclusions: We developed a SWL vs URS treatment choice SDA with promising content and face validity. Agreement and contradiction between content and face validation regarding relevance of anesthesia type and recovery time indicate further work is required to determine clinical utility and understand its potential ability to improve patient understanding and treatment satisfaction.
Source of Funding: Blue Cross Blue Shield of Michigan
Methods: The scope of the SDA was identified through discussions with patients, patient advocates and urologists in the Michigan Urological Surgery Improvement Collaborative (MUSIC). A steering committee consisted of patient advocates, MUSIC coordinating center, decision making content experts, biostatisticians and MUSIC urologists. Content domains were assessed through best available evidence and expert opinion. For content validation we conducted anonymous survey of 35 MUSIC urologists. Content Validity Ratios (CVR), numeric value indicating degree of expert validity, were calculated. Face validation interviews were conducted with patient advocates.
Results: A prototype using descriptive plain language and pictorial information was designed for nephrolithiasis patients who are candidates for SWL or URS. Page 1 addressed patient education and page 2 informed urologists of patient treatment goals. Six content domains were chosen: anesthesia type, effectiveness, number of procedures, risk, pain and recovery. 91.4% and 85.7% of urologists indicated that Page 1 and Page 2 accomplished their goals, respectively (Table 1). Anesthesia type was the only domain to receive a lower than acceptable CVR. Patient advocates reported high levels of face validation (Table 2).
Conclusions: We developed a SWL vs URS treatment choice SDA with promising content and face validity. Agreement and contradiction between content and face validation regarding relevance of anesthesia type and recovery time indicate further work is required to determine clinical utility and understand its potential ability to improve patient understanding and treatment satisfaction.
Source of Funding: Blue Cross Blue Shield of Michigan

.jpg)
.jpg)