Back
Poster, Podium & Video Sessions
Moderated Poster
MP28: Health Services Research: Practice Patterns, Quality of Life and Shared Decision Making III
MP28-06: National Trends in the Prescription of Narcotics in the Emergency Department in Patients with Nephrolithiasis
Saturday, May 14, 2022
1:00 PM – 2:15 PM
Location: Room 228
Spencer Liem*, Timothy Demus, Miami Beach, FL, Alexandra Perez, Fort Lauderdale, FL, Crystal Lee, Philadelphia, PA, Kevin George, Miami, FL, Alejandra Perez, Miami Beach, FL, Luigi Cubeddu, Fort Lauderdale, FL, Jorge Pereira, Miami Beach, FL

Spencer S. Liem, MD
Urology Resident
Mount Sinai Medical Center
Poster Presenter(s)
Introduction: In 2017, the Department of Health and Human Services (HHS) declared the opioid crisis a public health emergency. This study aims to describe the national changes in narcotic prescription and administration in the emergency department (ED) for patients with nephrolithiasis over a five-year period.
Methods: This is a retrospective cohort study using data collected from the National Hospital Ambulatory Medical Care Survey (NHAMCS) from ED visits from 2014 through 2018. Patients with nephrolithiasis were identified by using the respective ICD 9/10 codes. The primary study endpoint was the use of any opioid medication. Pre-declaration period was defined as 2014-2016 and post-declaration from 2017-2018. Chi-square test was used to examine the association of narcotic use pre/post declaration period, over the 5-year period. Estimates were adjusted to complex survey design using appropriate weight variables.
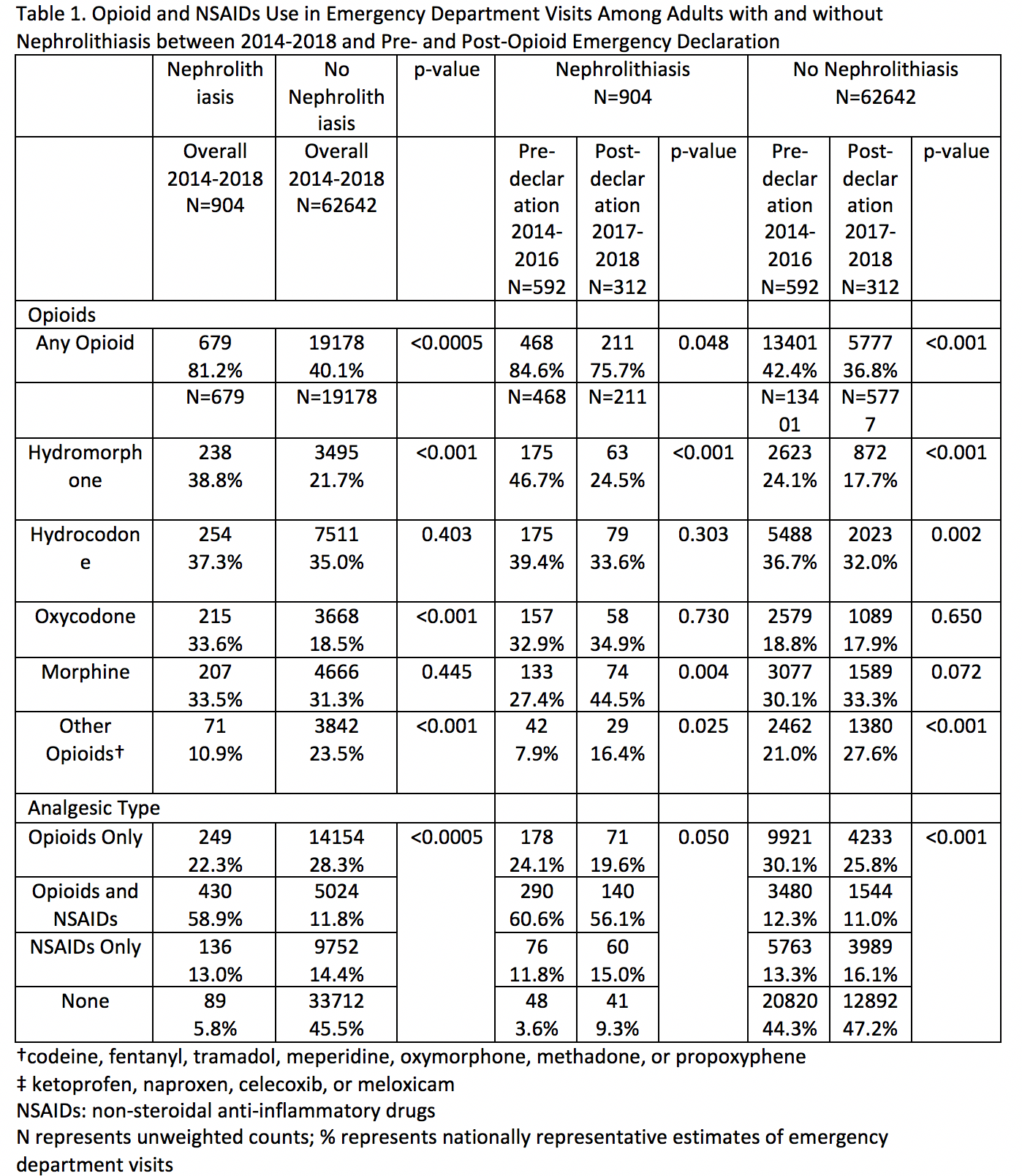
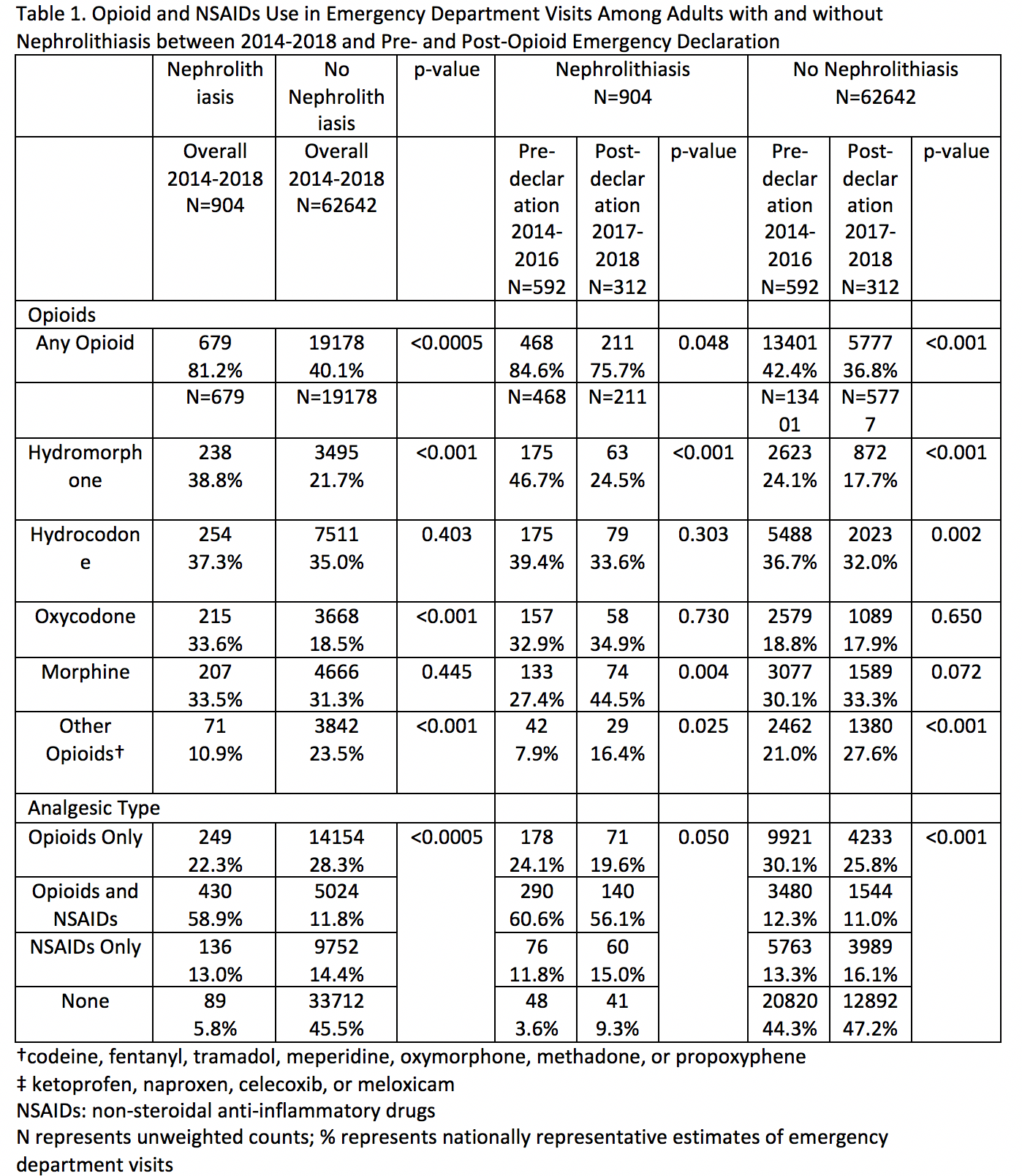
Results: 63,546 weighted (608,220,000 unweighted) individuals visited the ED from 2014-2018. 1.9% (1,207/63,546) had nephrolithiasis as a discharge diagnosis. Opioid narcotics were prescribed in 81.2% (679/904) of weighted patients with nephrolithiasis compared to 40.1% (19,178/62,642) in patients non-nephrolithiasis (P <0.0005) (Table 1). In the post-declaration era (2017-2018), 75.7% (211/311) of patients with nephrolithiasis were prescribed opioids, compared to 84.6% (468/592) of patients in the pre-declaration era (2014-2016), (p=0.048). In the post-declaration era, 36.8% (5,777/22,658) of patients with non-nephrolithiasis diagnosis were prescribed opioids while 42.4% (13,401/39,948) of patients in the pre-declaration era were prescribed opioids, (p < 0.001). In 904 unweighted visits with nephrolithiasis, opioids were prescribed in combination with NSAIDs in 58.9% (430/904) of visits. Opioids were the sole analgesic in 22.3% (249/904) of visits, while NSAIDs were the sole analgesic in 13.0%, (136/904).
Conclusions: Since the opioid crisis was declared a public health emergency, overall narcotic prescriptions have decreased, but prescription of narcotics in patients with nephrolithiasis in the emergency department have remained relatively unchanged. Increased efforts into narcotic prescribing stewardship may be beneficial in this higher risk patient population.
Source of Funding: NA
Methods: This is a retrospective cohort study using data collected from the National Hospital Ambulatory Medical Care Survey (NHAMCS) from ED visits from 2014 through 2018. Patients with nephrolithiasis were identified by using the respective ICD 9/10 codes. The primary study endpoint was the use of any opioid medication. Pre-declaration period was defined as 2014-2016 and post-declaration from 2017-2018. Chi-square test was used to examine the association of narcotic use pre/post declaration period, over the 5-year period. Estimates were adjusted to complex survey design using appropriate weight variables.
Results: 63,546 weighted (608,220,000 unweighted) individuals visited the ED from 2014-2018. 1.9% (1,207/63,546) had nephrolithiasis as a discharge diagnosis. Opioid narcotics were prescribed in 81.2% (679/904) of weighted patients with nephrolithiasis compared to 40.1% (19,178/62,642) in patients non-nephrolithiasis (P <0.0005) (Table 1). In the post-declaration era (2017-2018), 75.7% (211/311) of patients with nephrolithiasis were prescribed opioids, compared to 84.6% (468/592) of patients in the pre-declaration era (2014-2016), (p=0.048). In the post-declaration era, 36.8% (5,777/22,658) of patients with non-nephrolithiasis diagnosis were prescribed opioids while 42.4% (13,401/39,948) of patients in the pre-declaration era were prescribed opioids, (p < 0.001). In 904 unweighted visits with nephrolithiasis, opioids were prescribed in combination with NSAIDs in 58.9% (430/904) of visits. Opioids were the sole analgesic in 22.3% (249/904) of visits, while NSAIDs were the sole analgesic in 13.0%, (136/904).
Conclusions: Since the opioid crisis was declared a public health emergency, overall narcotic prescriptions have decreased, but prescription of narcotics in patients with nephrolithiasis in the emergency department have remained relatively unchanged. Increased efforts into narcotic prescribing stewardship may be beneficial in this higher risk patient population.
Source of Funding: NA

.jpg)
.jpg)