Back
Poster, Podium & Video Sessions
Moderated Poster
MP28: Health Services Research: Practice Patterns, Quality of Life and Shared Decision Making III
MP28-11: Implicit Bias in Communication of Risk in Prostate Cancer Treatment Consultations
Saturday, May 14, 2022
1:00 PM – 2:15 PM
Location: Room 228
Aurash Naser-Tavakolian*, Rebecca Gale, Michael Luu, Abhishek Venkataramana, Los Angeles, CA, Dmitry Khodyakov, Santa Monica, CA, Edwin Posadas, Howard Sandler, Jennifer Anger, Stephen Freedland, Brennan Spiegel, Timothy Daskivich, Los Angeles, CA

Aurash NaserTavakolian, MD
Cedars-Sinai Medical Center
Poster Presenter(s)
Introduction: A physician’s preference for treatment may bias the way that risk is communicated during prostate cancer treatment consultations. We sought to characterize the use of persuasive rhetorical devices when describing cancer prognosis, life expectancy, and side effects in relation to a physician’s recommendation for aggressive (surgery or radiation) or non-aggressive treatment.
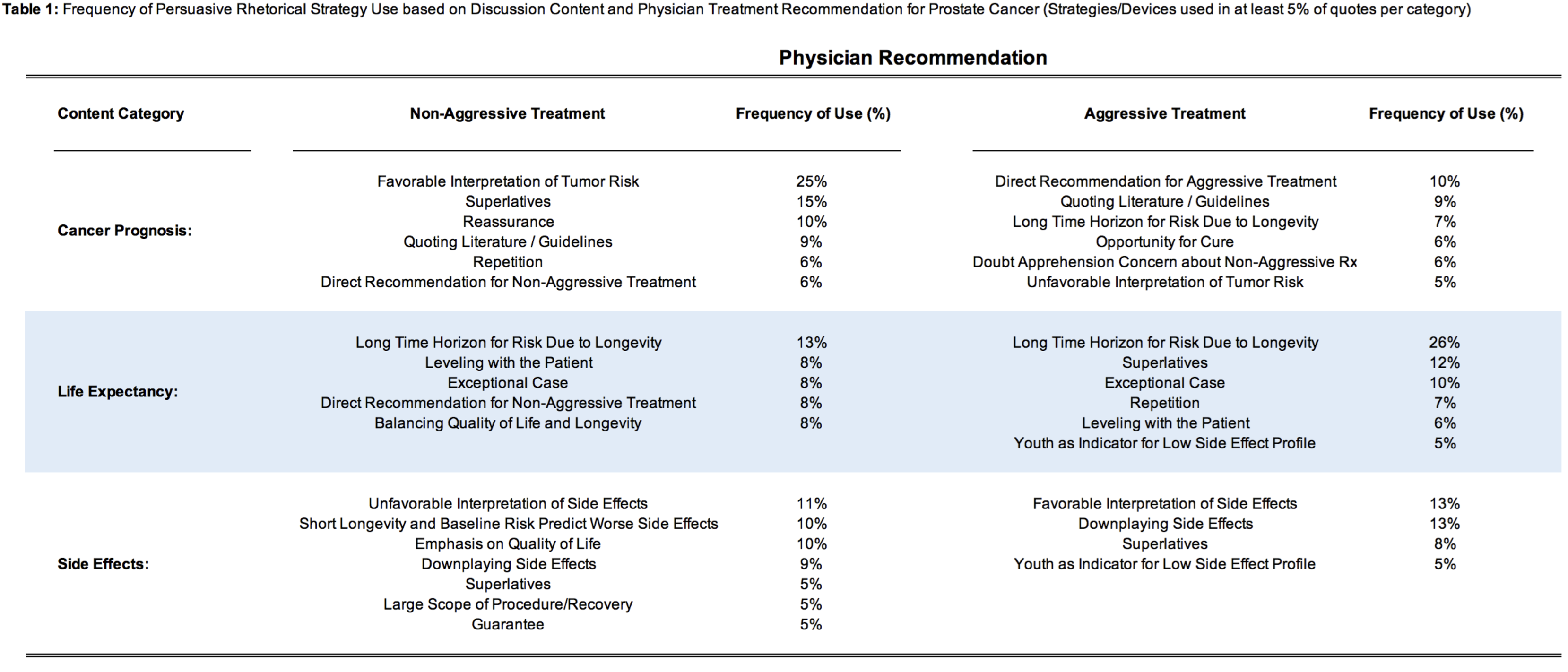
Methods: We transcribed treatment consultations of 40 men with non-metastatic prostate cancer across 10 multidisciplinary providers. Quotes pertaining to cancer prognosis, life expectancy, and treatment side effects were isolated. Coders were asked to identify rhetorical strategies favoring aggressive or non-aggressive treatment for each quote. Frequencies of rhetorical strategies were reported across content categories and treatment recommendations. Univariate logistic regression identified which rhetorical strategies were predictive of an aggressive or non-aggressive treatment recommendation.
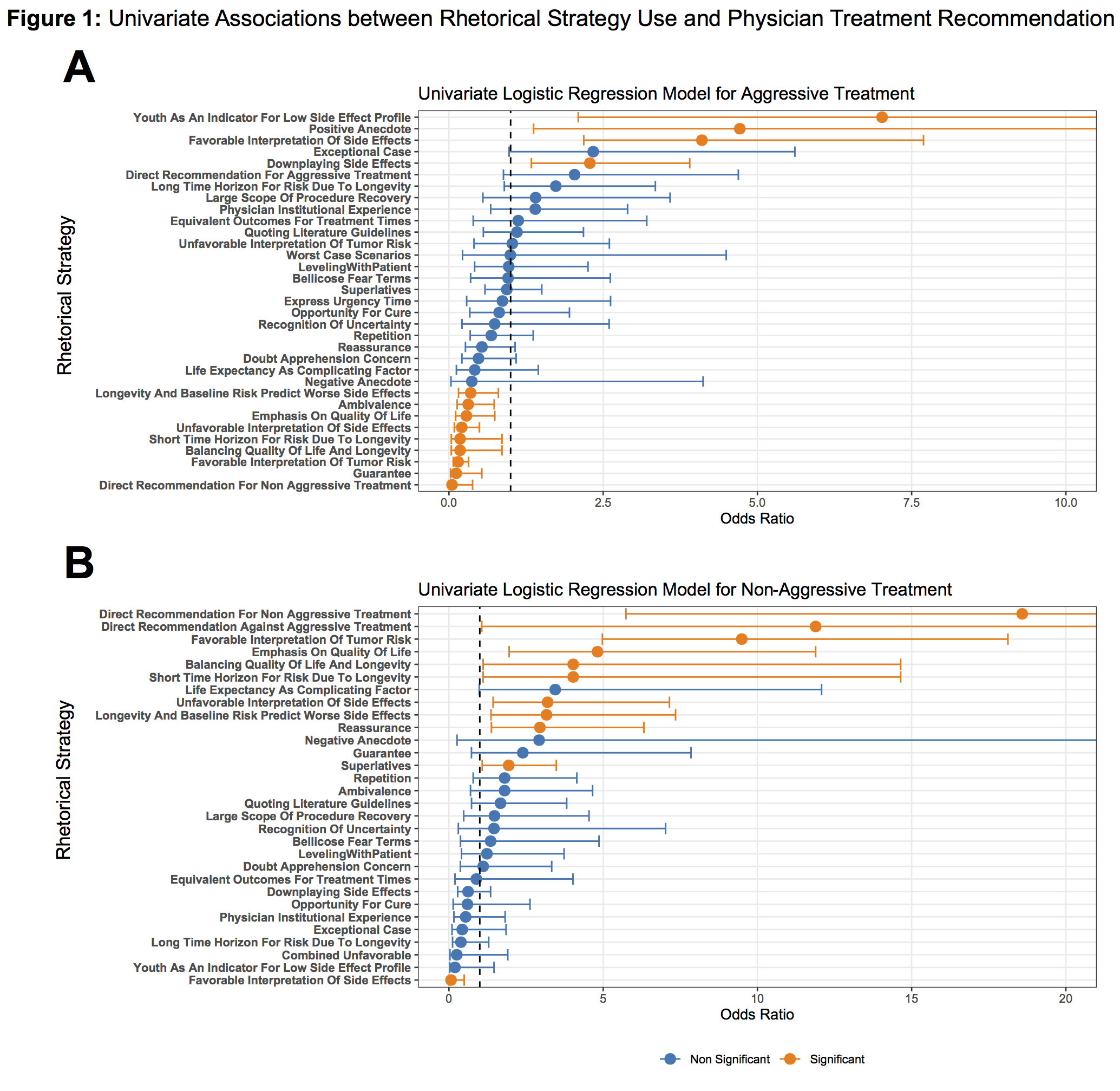
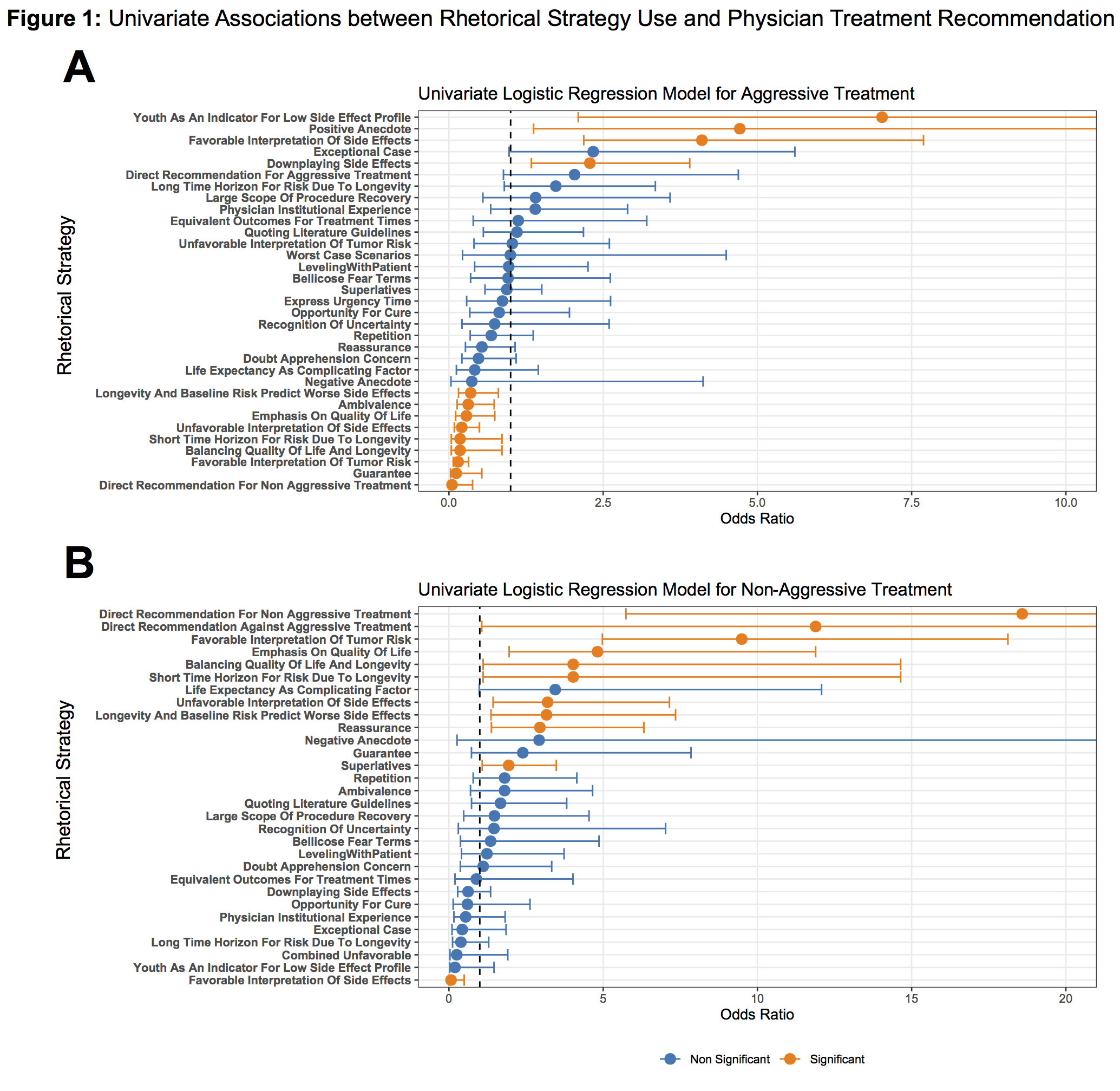
Results: Among 496 unique quotes, the most commonly used rhetorical strategies grouped by content category and treatment recommendation are shown in Table 1. In univariate logistic regression, significant predictors of an aggressive treatment recommendation included favorable interpretation of side effect data, youth as an indicator for low side effect profile, and downplaying side effects. Significant predictors of a non-aggressive treatment recommendation included direct recommendation, favorable interpretation of tumor risk data, unfavorable interpretation of side effect data, emphasis on longevity, and emphasis on quality of life (Figure 1).
Conclusions: A physician’s treatment preference appears to bias the way that risks of prostate cancer are reported. When favoring non-aggressive treatment, physicians amplify risks of side effects and downplay risk of cancer, while when favoring aggressive treatment, they downplay risks of side effects. Providers should be cognizant of potential biases when communicating risk in shared decision making.
Source of Funding: This work was supported by Career Development Award (K08 CA230155 to TJD) from the National Cancer Institute.
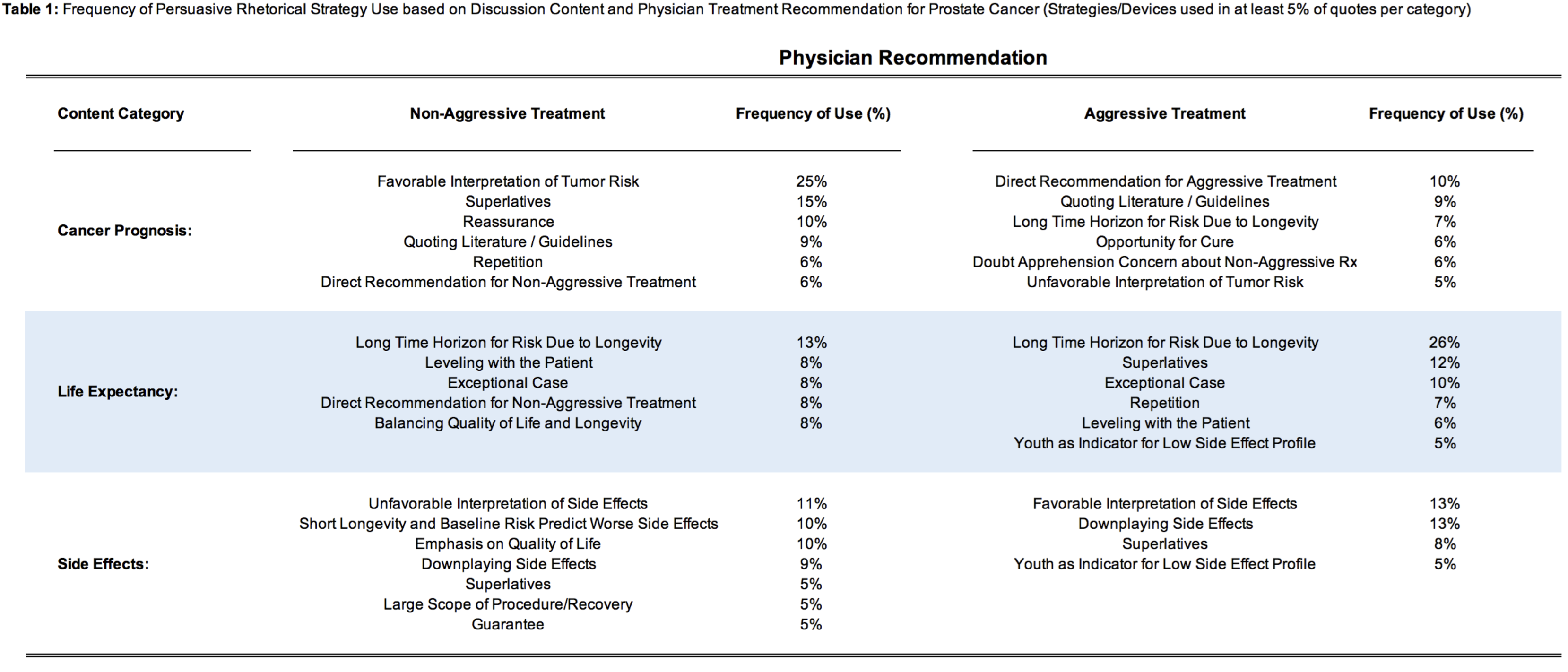
Methods: We transcribed treatment consultations of 40 men with non-metastatic prostate cancer across 10 multidisciplinary providers. Quotes pertaining to cancer prognosis, life expectancy, and treatment side effects were isolated. Coders were asked to identify rhetorical strategies favoring aggressive or non-aggressive treatment for each quote. Frequencies of rhetorical strategies were reported across content categories and treatment recommendations. Univariate logistic regression identified which rhetorical strategies were predictive of an aggressive or non-aggressive treatment recommendation.
Results: Among 496 unique quotes, the most commonly used rhetorical strategies grouped by content category and treatment recommendation are shown in Table 1. In univariate logistic regression, significant predictors of an aggressive treatment recommendation included favorable interpretation of side effect data, youth as an indicator for low side effect profile, and downplaying side effects. Significant predictors of a non-aggressive treatment recommendation included direct recommendation, favorable interpretation of tumor risk data, unfavorable interpretation of side effect data, emphasis on longevity, and emphasis on quality of life (Figure 1).
Conclusions: A physician’s treatment preference appears to bias the way that risks of prostate cancer are reported. When favoring non-aggressive treatment, physicians amplify risks of side effects and downplay risk of cancer, while when favoring aggressive treatment, they downplay risks of side effects. Providers should be cognizant of potential biases when communicating risk in shared decision making.
Source of Funding: This work was supported by Career Development Award (K08 CA230155 to TJD) from the National Cancer Institute.

.jpg)
.jpg)