Back
Poster, Podium & Video Sessions
Moderated Poster
MP29: Benign Prostatic Hyperplasia: Surgical Therapy & New Technology III
MP29-03: Is Simple Prostatectomy After Prior Minimally Invasive Surgical Therapies for Benign Prostatic Hyperplasia as Efficacious as Primary Simple Prostatectomy
Saturday, May 14, 2022
1:00 PM – 2:15 PM
Location: Room 225
Ram Pathak, Bridget Krol*, Nikhil Crain, Ashok Hemal, Winston-Salem, NC
Bridget Krol, BS
Wake Forest School of Medicine
Poster Presenter(s)
Introduction: Robotic simple prostatectomy (RSP) is indicated in patients with enlarged glands (>80 grams) who present with lower urinary tract symptoms (LUTS) attributed to benign prostatic hyperplasia (BPH). Salvage simple prostatectomy (SSP) is defined as any RSP performed for management of LUTS after failure of prior transurethral procedures. The aim of this study is to evaluate the efficacy of primary simple prostatectomy (PSP) versus SSP in ameliorating LUTS.
Methods: We retrospectively reviewed 117 patients who underwent RSP between 2013 and 2021. Indications for surgery were prostate glands (> 80g), bothersome LUTS, or symptoms refractory to medical management and/or previous prostate surgery. PSP and SSP preoperative patient characteristics, perioperative variables, and postoperative outcomes were recorded for comparison. The severity of LUTS was assessed using the International Prostate Symptom Score (IPSS). Two-tailed Student’s t-tests were performed to compare primary vs. salvage RSP cohorts at a p-value (p) of 0.05.
Results: Of 117 patients who underwent RSP, 95 were primary and 22 were in the salvage setting with 15 undergoing prior TURP, 3 status post TUMT, 1 status post vaporization, 1 status post nodal ablation, and 2 status post UroLIFT. Mean length of stay following RSP was 1.91 (days). At mean follow up 12.26 (months), none of the patients required re-operation for LUTS. Preoperative IPSS for primary and salvage RSP was 18.69 and 17.31, respectively (p=0.63) and postoperative IPSS for primary and salvage RSP was 5.68 and 7.33, respectively (p=0.63).
Conclusions: Regardless of primary or salvage indication, RSP remains a highly efficient and durable procedure for maximum improvement to a patient’s voiding symptomatology and should be considered the standard approach for tackling enlarged prostate glands with or without concomitant pathology. The postoperative functional outcomes are excellent with many patients resolving the need for chronic catheterization. RSP performed in the salvage setting greatly improved urinary function outcomes in patient’s after failure of previous transurethral procedures to treat LUTS.
Source of Funding: None
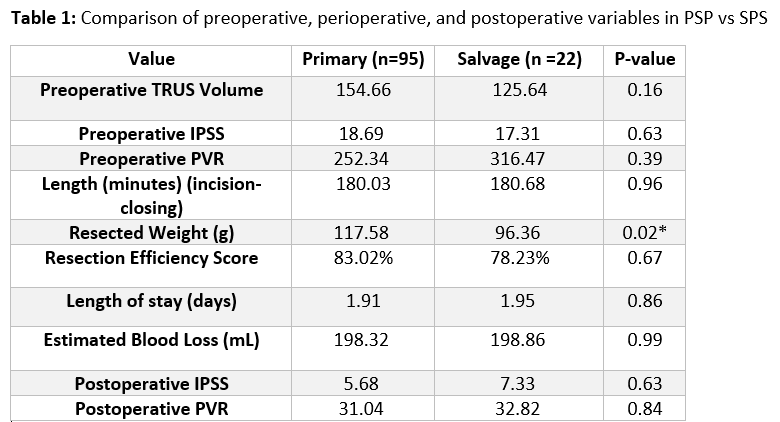
Methods: We retrospectively reviewed 117 patients who underwent RSP between 2013 and 2021. Indications for surgery were prostate glands (> 80g), bothersome LUTS, or symptoms refractory to medical management and/or previous prostate surgery. PSP and SSP preoperative patient characteristics, perioperative variables, and postoperative outcomes were recorded for comparison. The severity of LUTS was assessed using the International Prostate Symptom Score (IPSS). Two-tailed Student’s t-tests were performed to compare primary vs. salvage RSP cohorts at a p-value (p) of 0.05.
Results: Of 117 patients who underwent RSP, 95 were primary and 22 were in the salvage setting with 15 undergoing prior TURP, 3 status post TUMT, 1 status post vaporization, 1 status post nodal ablation, and 2 status post UroLIFT. Mean length of stay following RSP was 1.91 (days). At mean follow up 12.26 (months), none of the patients required re-operation for LUTS. Preoperative IPSS for primary and salvage RSP was 18.69 and 17.31, respectively (p=0.63) and postoperative IPSS for primary and salvage RSP was 5.68 and 7.33, respectively (p=0.63).
Conclusions: Regardless of primary or salvage indication, RSP remains a highly efficient and durable procedure for maximum improvement to a patient’s voiding symptomatology and should be considered the standard approach for tackling enlarged prostate glands with or without concomitant pathology. The postoperative functional outcomes are excellent with many patients resolving the need for chronic catheterization. RSP performed in the salvage setting greatly improved urinary function outcomes in patient’s after failure of previous transurethral procedures to treat LUTS.
Source of Funding: None

.jpg)
.jpg)